Mammography is useful in discovering tumors too small to be felt. The procedure involves taking an X-ray of the breast with a very low radiation dose. It has been shown that there is little risk from the exposure for women over 35 who have annual mammograms. However, for younger women who are at high risk for breast cancer due to their BRCA status, exposure to X-rays may lead to an increase in risk.1
Patients should verify that their clinic is FDA certified and specializes in mammography or processes a large number of mammograms. Visit the FDA to verify that your local facility is accredited. Most health plans, Medicare, and Medicaid cover part or all of the costs of mammography. The American Cancer Society has information about low cost mammograms available in most areas.2.
Topics on this page:
- Mammography Screening Guidelines
- What to Expect
- Results of a Mammography
- Digital Mammography
- Mammography After Mastectomy
- Mammography After Breast Augmentation
- Frequently Asked Questions About Mammography
- Know the Flow: Mammography
Watch a documentary about mammography
Mammography Screening Guidelines
Recommendations for screening mammograms have been revised throughout the years to reflect new data that have been collected on the pros and cons of screening mammograms. Mammograms can save lives, but they can also lead to false positive diagnoses and unecessary and potentially harmful treatments, such as surgery, radiation, and chemotherapy. The following chart contains 4 key groups' recommendations for screening mammograms. Differences between the groups' recommendations may be due to differences in the methods by which each group balances the pros and cons of screening mammograms.
| When to start getting mammograms | Frequency of testing for average risk individuals | When to stop getting mammograms
| |
US Preventative Services Task Force | Age 50 | Biennially (once every other year) | Age 74 |
American Cancer Society | Age 45 | Once every year until age 55, then once every other year | Not defined. Continue with mammography screenings as long as individual is in good overall health and has a life expectancy of at least 10 more years |
American College of Radiology | Average risk individuals: age 40 High risk individuals: by age 30, but not before age 25 | Annually | Not defined. Continue with mammography screenings as long as individual is in good health |
American Congress of Obstetricians and Gynecologists | Age 40 | Annually | Not defined. |
What to Expect
The patient will first be requested to undress above the waist, and put on a provided wrap. A technician will then help position the breast for the mammogram. If the sex of the technician is of concern, inquiries should be made prior to the visit. A normal screening mammogram involves taking two views of each breast, and the whole procedure lasts about 20 minutes. The process involves the brief, a few seconds long, compression of the breasts. This is done to obtain the best possible image of all breast tissue. The compression may be uncomfortable, but if there is pain the technician and physician should be notified. To lessen discomfort and pain, it is suggested that patients avoid scheduling mammograms for the week before or during menstruation when breasts may be more sensitive. Also, it is suggested not to wear deodorant, powder, or cream under the arms so as not to interfere with the quality of the mammogram.2 The image below is a labeled representation of a mammography machine.

Results of a Mammography
The radiologist who reads the mammograms has a difficult job because the normal appearance of the breasts is different for each woman. For this reason, it is valuable to have previous mammograms available for comparison. Therefore, if mammographies are scheduled at different locations, the patient should make sure that the new facility has access to any previous mammograms. Mammography does not directly detect cancer. Instead, it is used to detect possible abnormalities, which can then be checked by a biopsy to determine if the changes are cancerous or benign. Depending on the radiologists' interpretation of an abnormality, the patient may be asked back for more diagnostic mammograms, for a follow up mammogram in 3-6 months, ultrasound, and/or biopsy. A common finding on mammogram is a cyst (a benign collection of fluid in the breast). The way to determine if a detected abnormality is a cyst is through an ultrasound examination or by needle aspiration.2
On the mammogram, there are two principal signs of cancer: calcifications and/or the presence of a mass. Calcifications (deposits iof calcium compounds in the breast) show up as white spots on a mammogram and occur in two forms, microcalcifications and macrocalcifications. Macrocalcifications tend to be large and coarse looking and are associated with aging. They are common in women over 50, and are present in a small percentage of younger women. Macrocalcifications are not typically associated with cancer. Microcalcifications are smaller and are considered a sign of possible malignancy, even without a visible mass. The radiologist must interpret the characteristics of the mass to determine the possibility of cancer, and will order diagnostic tests and possibly a biopsy.2
The image on the left shows the mammogram of a normal breast, while the image on the right shows a mammogram with an abnormality detected (denoted by the red arrows). Click on the images to visit their source, the Breast Center of St. Louis University.
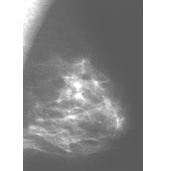
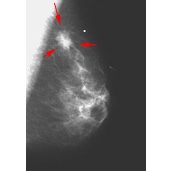
Requests for additional testing does not necessarily mean there is anything to fear. The clincians may call a patient back just because something looks a little suspicious and they would like to make a more thorough examination. In the event that a biopsy is indicated the likelihood of cancer is still small. Only 8-10% of those called back will need a biopsy, and approximately 20% of those will be diaganosed as having some form of cancer.2
Women with denser breasts show a decreased mammographic sensitivity, meaning it is harder to interpret the x-rays films and to see all of the breast tissue clearly. Ultrasound has been considered as an alternative to or supplementary to mammography for women with dense breasts because it can more effectively screen all of the breast tissue.7 However, ultrasound is not effective in detecting microcalcifications, which are an early sign of possible breast cancer.2
Digital Mammography
Digital mammography is a relatively new way of capturing the mammographic images. Instead of using X-ray film to capture the image, computerized sensors collect the image.
Digital mammography is becoming more popular because the images are stored on a computer and may be read by a radiologist directly on a computer screen. Mammograms can be shared with other physcians more easily via computer than by hand. Importantly, radiologists can enhance the images to get a better view of particular areas.2
Below is a comparison of images from a regular mammogram (on the left) and an enhanced digital mammogram (on the right). The digital mammogram allowed for the discovery of an otherwise undetectable abnormality. Currently there is debate in the field as to whether the increased detection of cancer by digital imaging justifies its increased cost to the patient. A fear is that increased cost could prevent some women from having mammography screening.

Images courtesy of Memorial Sloan-Kettering Cancer Center
A study published in 2012 showed that digital mammography was better than film mammmography at detecting 'high grade' ductal carcinoma in situ (DCIS). This is the type of pre-cancerous change that is most likely to advance to invasive cancer.8
Mammography After Mastectomy
Treatment for breast tumors may not involve a complete mastectomy. A Breast Conserving Treatment (BCT) such as a lumpectomy (the removal of the tumor and a margin of normal tissue surrounding it) may be utilized in conjunction with radiation and/or chemotherapy. In this case, it is suggested that the patient have a mammogram of the affected breast six months after completion of treatment because radiation and chemotherapy can alter the normal view of breasts on mammograms. The radiologist can then use this image as a baseline to compare with any future images. Opinions differ on the optimum frequency of mammography after treatment. The decision is one to be made by the physician and patient.2
If a total, modified radical, or radical mastectomy has been performed, mammograms are unnecessary for that breast. Also, if reconstruction was performed afterwards with implants or muscle tissue, regular mammograms are not usually taken. The unaffected breast should still be screened according to normal standards. Patients who have undergone a subcutaneous mastectomy (one in which the nipple and tissue just under the skin are retained) require regular screening of the affected breast.2
Mammography After Breast Augmentation
Women with breast implants require regular breast cancer screening. Implants may interfere with mammography and can prevent the imaging of some breast tissue. As a result, four more x-ray films, called implant displacement views, must be taken. In these views, the implant is pushed toward the chest wall. The type of implants that cause the least interference with mammography are those placed behind the chest muscle. Mammograms do not cause implants to rupture and they usually cannot detect a rupture. MRI may be used to detect ruptures in breast implants.2
Frequently Asked Questions About Mammography
BSE stands for Breast Self-Exam. Initially, BSE were thought to be a good screening tool for breast cancer, but it was later shown that BSE led to additional women having to undergo a biopsy but was not shown not improve cancer survival.9
Know the Flow: Mammography
Know the Flow is an educational game for you to test your knowledge. To play:
- Drag the appropriate choices from the column on the right and place them in order in the boxes on the left. Note that you will only use five of the six choices to complete the game.
- When done, click on 'Check' to see how many you got correct.
- For incorrect answers, click on 'Description' to review information about the processes.
- To try again, choose 'Reset' and start over.
Please visit us on a larger screen to play this game.
- 1 Mettler FA, Upton AC, Kelsey CA, Ashby RN, Rosenburg RD, Linver MN. "Benefits Versus Risks from Mammography: A Critical Reassessment." Cancer (1996). 77(5): 903-909. [PUBMED]
- 2abcdefghij "Mammography and Other Breast Imaging Procedures." American Cancer Society (6-19-2002). [http://www.cancer.org/Healthy/FindCancerEarly/ExamandTestDescriptions/MammogramsandOtherBreastImagingProcedures/mammograms-and-other-breast-imaging-procedures]
- 3 Final Recommendation Statement: Breast Cancer: Screening. U.S. Preventive Services Task Force. [http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/breast-cancer-screening]
- 4 Oeffinger KC, Fontham ET, Etzioni R, Herzig A, Michaelson JS, Shih YC, Walter LC, Church TR, Flowers CR, LaMonte SJ, Wolf AM, DeSantis C, Lortet-Tieulent J, Andrews K, Manassaram-Baptiste D, Saslow D, Smith RA, Brawley OW, Wender R; American Cancer Society. Breast Cancer Screening for Women at Average Risk: 2015 Guideline Update From the American Cancer Society. JAMA. 2015 Oct 20;314(15):1599-614. doi: 10.1001/jama.2015.12783. [PUBMED]
- 5 The American College of Radiology. ACR PRACTICE PARAMETER FOR THE PERFORMANCE OF SCREENING AND DIAGNOSTIC MAMMOGRAPHY. [http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/Screening_Mammography.pdf]
- 6 https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2017/07/breast-cancer-risk-assessment-and-screening-in-average-risk-women
- 7 Whitman GJ. "The Role of Mammography in Breast Cancer Prevention." Current Opinion in Oncology (1999). 11(5): 414. [PUBMED]
- 8 Bluekens AM, Holland R, Karssemeijer N, Broeders MJ, den Heeten GJ. Comparison of Digital Screening Mammography and Screen-Film Mammography in the Early Detection of Clinically Relevant Cancers: A Multicenter Study. Radiology. 2012 Oct 2. [Epub ahead of print] [PUBMED]
- 9 Kosters JP, Gotzsche PC. Regular self-examination or clinical examination for early detection of breast cancer (review). Cochrane Database Syst Rev. Issue 3: CD003373, 2008. [View Cochrane Report on Breast Self Examination]