The main kinds of cancer treatments are introduced briefly on this page and described in detail in their respective sections.
Contents on this topic:
- Introduction to Cancer Treatments (this page)
- A Graphical Guide To Cancer Treatment An illustrated overview of the main cancer treatments.
- Biological Therapies These treatments are designed to help a patient's natural defenses fight cancer.
- Bone Marrow Transplantation (BMT) Bone marrow transplantation is done to treat blood cell cancers.
- Chemotherapy Chemotherapy is a term for many different drugs used to treat cancer.
- Cryotherapy (Cryoablation) In cryotherapy, tumors are frozen, killing the cancer cells
- Hormonal Treatments The growth of some cancers is caused by hormones, signals normally produced by the body. These treatments block/prevent the signals.
- Immunotherapy These treatments are designed to overcome the immune system blocks created by cancer cells.
- Radiation Therapy Radiation causes damage to cells, and when directed at tumors, can kill cancer cells.
- Radiofrequency Ablation Beams of energy cause cancer cells to heat up and die. The beams are NOT the same as those used in radiation therapy.
- Surgery Many tumors can be removed surgically.
- Targeted Therapies These treatments are designed to attack defects found in cancer cells, but not in normal cells.
- Vaccines to Treat Cancer Vaccines are used to 'show' the body's defenses what should be attacked, in this case - cancer cells.
- Cancer Treatment Tables
- Interactive Game: The Grid
Related content: The Drug Discovery and Development Process Cancer drugs take years to make their way to patients. Learn where cancer drug candidates come from and how they become drugs.
Introduction to Cancer Treatments
The treatment given for cancer is variable and dependent on a number of factors including the type, location and amount of disease, and the health status of the patient. Most treatments are designed to either directly kill/remove the cancer cells or to lead to their eventual death by depriving them of signals needed for survival. Other treatments work by stimulating the body's own defenses against the cancer cells.
There are three general types of cancer treatments:
- radiation therapy (delivered by a radiation oncologist);
- surgery (performed by a surgical oncologist)
- systemic therapy (usually administered by a medical oncologist)
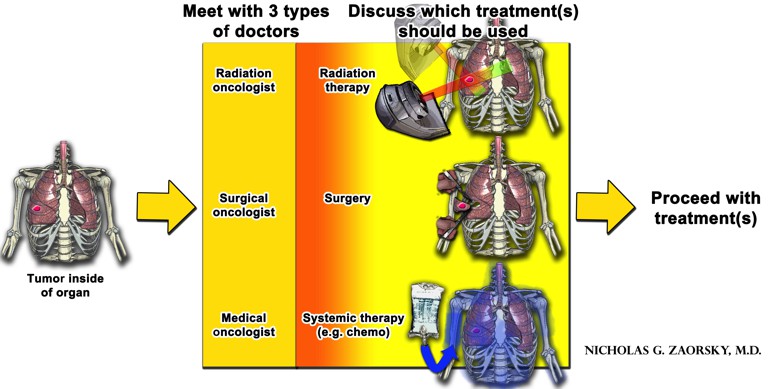
The goal of any treatment is to kill as many cancer cells as possible and and minimize the death of normal cells. Each type of treatment has advantages and disadvantages. In most cancers, multiple treatment options must be used together (either at the same time, or one after the other) to get the best results.
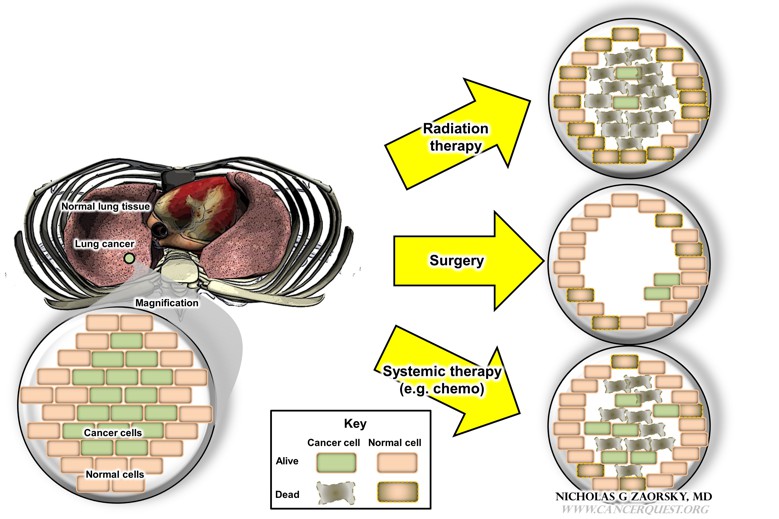
This figure compares the advantages and disadvantages of the three types of cancer treatment options. In the left panel, a patient has a lung cancer; in the magnification below, there are cancer cells (in green) and normal cells from surrounding tissues (in this case, lung). The magnification is not drawn to scale. The effects of each treatment (radiation, surgery, systemic therapy) are illustrated on the right; note that there are important differences in how these treatments affect the cancer cells and the patient (described below).
Radiation therapy
With radiation therapy, 3D models are created of the tumor and the surrounding normal area. Radiation therapy is focused on the tumor, and the normal tissues are avoided (akin to a magnifying glass focusing light).
The advantages of radiation therapy include:
- death of a large proportion of cancer cells within the entire tumor (radiation alone may be used to cure some small tumors)
- death of microscopic disease, very small groups of cancer cells that would not be visible to the naked eye (e.g. at the time of surgery)
- ability to shrink tumors (which may help to relieve mass effect (the pushing of a tumor on nearby body parts); or it may be done before surgery to shrink tumors to a size that makes them treatable with surgery (resectable).
- relative safety for the patient (radiation can be delivered from outside of the body and focused on the tumor, is painless, and generally does not require anesthesia)
- works to make systemic therapy more effective (i.e. the ability to kill more cells together than either therapy could do alone)
- organ preservation (e.g. not removing a breast, larynx, or part of the gastrointestinal tract, which would have significant negative impact on a patients quality of life
- stimulation of an immune response against the tumor
The disadvantages of radiation therapy include:
- damage to surrounding tissues (e.g. lung, heart), depending on how close they are to the tumor
- inability to kill tumor cells that cannot be seen on imaging scans and are therefore not always included on the 3D models used to plan the radiation This can include cancer in near-by lymph nodes or cancer that has spread to distant locations (metastatic disease).
- inability to kill the all cancer cells in tumors. This is more likely with large tumors.
- inability to relieve mass effect in certain parts of the body (e.g. brain). This can lead to the need for surgery.
- poor killing of cancer cells in areas that do not have a good supply of oxygen (e.g. in an area after surgery; in a limb with a poor blood supply)
- increased incidence in wound complication and poor healing (e.g. if surgery is used after radiation; or in parts without good circulation)
- inconvenience of radiation therapy (e.g. in some cases it must be delivered daily, 5 days per week, for 1-2 months)
Surgery
For much of human history, surgery was the first line of treatment for many solid tumors. With surgery, a patient is taken to the operating room, put under anesthesia, and the tumor removed. For some cancers, the entire tumor can not be removed, but some of it can be removed, a process called debulking. Benign growths may also be removed.
The advantages of surgery include:
- the removal of a large volume of tumor can relieve mass effect, which may reduce symptoms instantly
- the removal of cancer cells that are producing blood-borne factors that stimulate the growth of cancer cells in other parts of the body
- the removal of a tumor in a part of the body that cannot be treated with radiation (e.g. if the patient has already received radiation there) or systemic therapy (e.g. in the brain, where certain chemotherapy cannot reach)
- potential ability to remove all cancer cells in a small area (the patient may be cured with surgery alone)
- ability to look at the cancerous tissue (pathology).
- Tissue samples can be examined to decide the best treatment options for that particular patient.
- If the patient has already been treated, the samples can be used to see how the cancer responded to previous treatment to see if more of that treatment should be given or if the treatment needs to be changed.
- convenience for the patient (since the surgery is performed once over the course of a day while the patient is asleep)
The disadvantages of surgery include:
- inability to kill microscopic disease around the edges of the tumor may leave tumor cells in the patient after surgery.
- the patient must be able to tolerate the surgery and anesthesia (i.e. have minimal medical problems, have good lung function, not be on certain medications)
- some damage to nearby normal tissues (e.g. removing ribs or normal lung tissue to reach a lung tumor)
- complications from surgery (e.g. infection, and others that are site-specific)
- inability to remove cancer in other parts of the body (i.e. metastatic disease)
- inability to safely remove kill cells in certain parts of the body where radiation therapy may have less side effects (e.g. in certain types of brain tumors)
- removal of an organ which may affect the patients quality of life (e.g. breast, larynx, bowel)
- inability of a surgeon to discern cancer cells from normal cells with the naked eye (particularly after chemotherapy or radiation have been delivered to the site)
Systemic therapy
Systemic therapy includes medications that affect the entire body (e.g. hormones, chemotherapy, targeted therapy, antibodies, vaccines, biological response modifiers, integrative oncology, immune-modulators).
The advantages of systemic therapy include:
- the ability to kill many cancer cells throughout the entire body (including cancer cells in the main tumor, and other tumors in the body)
- work together with radiation therapy (i.e. can kill more cells together than either therapy could do alone
- ability to kill microscopic disease at the edge of the main tumor that may not be seen by the naked eye of a surgeon (thereby decreasing the chance that therecancer cells will be left behind at the time of surgery)
- tailoring of the systemic treatment for each patient (e.g. specific hormonal therapies for breast cancers; targeted therapies for lung cancers), a backbone of personalized medicine
- preservation of an organ (e.g. not removing a breast, larynx, or part of the gastrointestinal tract, which would have significant negative impact on a patients quality of life)
The disadvantages of systemic therapy include:
- inability to kill a tumor alone (in most cases, systemic therapy must be used with either surgery or radiation therapy)
- inability to deliver systemic therapy if the patient is on certain medications (e.g. blood thinners), or around the time of surgery, or has certain medical conditions (e.g. kidney failure, liver failure, heart disease)
- systemic toxicities (since the therapies go through the entire body and may affect all normal tissues) The side-effects are therapy-dependent and can be different for different drugs
- inability of the systemic therapy to get to the tumor (e.g. crossing the blood-brain barrier; going to a limb where there is poor circulation)
- relatively uneven killing of cancer cells in tumors (akin to having hundreds of beach balls and randomly popping half of them — one does not know where the remaining beach balls [the living cancer cells] are still located;
- relative inconvenience of systemic therapy (e.g. some forms of chemotherapy must be delivered daily, 5 days per week, for weeks; or they must be taken orally for years).
Learn how cancer drugs are discovered and developed.
To find information on a specific cancer drug or treatment, you may search the site using the search tool at the top of the page and proceed directly to the most relevant pages for the treatment of interest.
The Food and Drug Administration (FDA) is responsible for approving drugs that can be used by oncologists to treat cancer and also evaluates drugs or other products that may be able to reduce the risk of cancer.
Visit an FDA page to see a list of drugs that have been approved recently. The drugs approvals are listed by date and you can view more information about any approved item.
Learn more about the FDA Office of Hematology and Oncology Products.
If you find the material useful, please consider linking to our website