Sections discussed on the following page:
- What is a PSA Test?
- Normal PSA Values
- Interpretation pf PSA Test Results
- Testing Recommendations
- Understanding the Results
- New Technologies
What is a PSA Test?
The prostate specific antigen (PSA) is a glycoprotein produced by prostate cells and is a normal component of semen.1
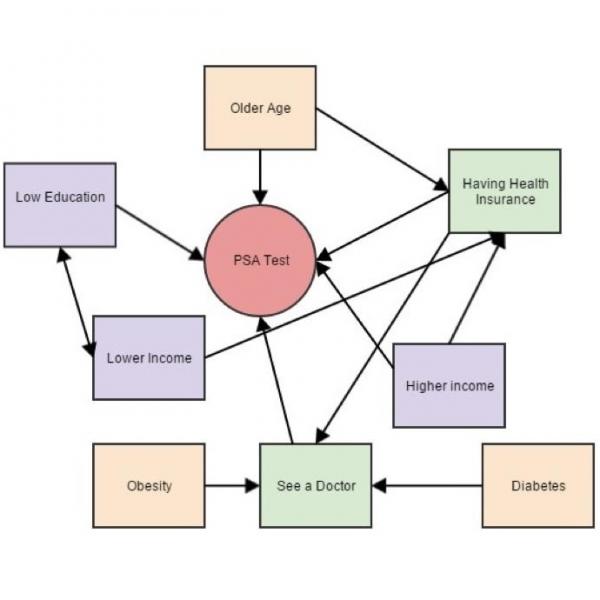
When abnormal events occur in the prostate, such as prostate cancer, the overabundance of prostate cells, the overproduction of PSA, or the leaking of PSA into the bloodstream may result in a measurable increase in the level of PSA in the blood. Blood test are used to assess the level of PSA in the blood. A higher-than-normal level of PSA might indicate a problem with the prostate, including, but not limited to, cancer.
There is an ongoing debate about the need for annual PSA tests. Be sure to discuss your need for a PSA test with your healthcare provider.2 3
Normal PSA Values
In general, a PSA level less than 4 ng/ml is considered normal, and greater than 10 ng/ml is considered high. Levels between 4 and 10 ng/ml represent a grey area in which a doctor may consider a digital rectal exam before recommending further testing.1
Interpretation of PSA Test Results
The interpretation of PSA levels is not straightforward. Elevated PSA levels indicate something has caused more PSA than usual to enter the bloodstream from the prostate, but the test is not able to identify the cause of the elevation. Several factors can cause a rise in PSA levels, such as a prostate infection or benign enlargement of the prostate.1
Many men with elevated PSA levels DO NOT have prostate cancer. Additionally, not all prostate cancers cause PSA levels to rise. These cancers would not be detected by the PSA test. Prostate cancer, unlike many other cancers, often grows slowly, and does not always pose a significant health risk. Some prostate cancers do grow quickly, but neither the PSA test nor any available test today can differentiate between slow and fast growing prostate cancers. While some people will benefit from having the PSA test, patients should discuss the benefits and limitations of this test with their health care provider before having it performed and when interpreting the results.
Testing Recommendations
Because PSA test results are so difficult to interpret, the benefit of routine screening is not completely clear. For this reason,there is disagreement among cancer organizations about who should be tested and when they should be tested. The opinions of two of the major organizations involved in the debate are presented below as exact quotes. The American Cancer Society statement was released first and is therefore presented first.
The American Cancer Society published guidelines in 2010 state: "The American Cancer Society (ACS) recommends that men have a chance to make an informed decision with their health care provider about whether to be screened for prostate cancer. The decision should be made after getting information about the uncertainties, risks, and potential benefits of prostate cancer screening. Men should not be screened unless they have received this information. The discussion about screening should take place at age 50 for men who are at average risk of prostate cancer and are expected to live at least 10 more years. This discussion should take place starting at age 45 for men at high risk of developing prostate cancer. This includes African Americans and men who have a first-degree relative (father, brother, or son) diagnosed with prostate cancer at an early age (younger than age 65). This discussion should take place at age 40 for men at even higher risk (those with several first-degree relatives who had prostate cancer at an early age). After this discussion, those men who want to be screened should be tested with the prostate specific antigen (PSA) blood test. The digital rectal exam (DRE) may also be done as a part of screening."4
In response to the ACS guidelines, the American Urological Association (and the AUA Foundation) published documents that state their position: "Prostate cancer testing is an individual decision that patients should make together with their doctor. The AUA believes that all men, with a life expectancy of 10 years or more, should have a baseline PSA test at the age of 40. Physicians should determine rescreening intervals for each patient based on PSA (and, on occasion on its change over time). Likewise, the decision to proceed to prostate biopsy should be based not only on elevated PSA and/or abnormal DRE results, but should take into account multiple factors including free and total PSA, patient age, PSA velocity, PSA density, family history, ethnicity, prior biopsy history and comorbidities. Although prostate cancer risk correlates with serum PSA, there is no PSA value below which a man may be reassured that he does not have biopsy detectable prostate cancer."5
These two organizations do agree on is that men should talk with their doctors about the benefits and risks of PSA testing.
In 2018, the U.S. Preventive Services Task Force (USPSTF) released PSA screening recommendations for two age groups. For men between the ages of 55 and 69 years old, the decision to undergo PSA screening for prostate cancer should be an individual one, after weighing out the potential benefits and and harms with their physicians. For men aged 70 years and older, the USPSTF recommends against PSA screening for prostate cancer.6
A study done to predict what would happen to the number of cases of metastatic prostate cancer in the U.S. each year if the PSA test was no longer used. There results predict that there would be 3x as many cases of metastatic prostate cancer detected per year (about 25,000 instead of about 8,000) if the PSA test was no longer used at all.7
It is important to understand exactly what an elevated PSA means. An elevated PSA level may indicate a higher risk of prostate cancer, but many men with elevated PSA levels do not have cancer. Importantly, many men with early-stage prostate cancer will not have elevated PSA levels.8 9
A digital rectal exam along with a PSA test can help a doctor assess the prostate further, but it still may not be enough to diagnose cancer. A physician may schedule a biopsy following an elevated PSA level along with a suspicious digital rectal exam. A biopsy is the removal of a small sample of the prostate for microscopic examination. Biopsy is the only way to confidently diagnose prostate cancer.
Newer technologies are being employed in an effort to make the PSA level test more accurate. Scientists are looking at whether a specific form of PSA, called free-PSA, is better at predicting the presence of cancer than total PSA.10 In 1998, the FDA approved the use of free-PSA to help better-diagnose men with PSA levels between 4 and 10 ng/ml (the "grey zone"). In general, lower levels of free-PSA are associated with an increased possibility of having cancer. While the free-PSA test can make the regular PSA test more specific, it is still not perfect. Other techniques visualize the prostate using ultrasound, and use this information to supplement the PSA test. Finally, some scientists believe that the rate at which PSA levels increase may be useful in distinguishing prostate cancer from other changes in the prostate.11
For more information about prostate cancer diagnosis and staging visit the Winship Cancer Institute of Emory University.
- 1 a b c American Foundation for Urological Disease [http://www.afud.org/conditions/psa.html]
- 2Kell JS. Prostate-specific antigen tests and prostate cancer screening: an update for primary care physicians. Can J Urol. 2010 Feb;17 Suppl 1:18-25. [PUBMED]
- 3Loeb S, Catalona WJ. Prostate-specific antigen screening: pro. Curr Opin Urol. 2010 May;20(3):185-8. [PUBMED]
- 4American Cancer Society Guidelines for Prostate Cancer Early Detection. Accessed October 3, 2010 [http://www.cancer.org/Cancer/ProstateCancer/MoreInformation/ProstateCancerEarlyDetection/prostate-cancer-early-detection-a-c-s-recommendations]
- 5American Urological Association website. PSA testing response PDF. Accessed August 25, 2010 [http://www.urologyhealth.org/pdfs/AUA_ACS_Response.pdf]
- 6. (2018). Screening for Prostate Cancer: US Preventive Services Task Force Recommendation Statement. Jama, 319(18), 1901-1913. http://doi.org/10.1001/jama.2018.3710 (Original work published December 2018) [PUBMED]
- 7Scosyrev E, Wu G, Mohile S, Messing EM.Prostate-specific antigen screening for prostate cancer and the risk of overt metastatic disease at presentation: Analysis of trends over time. Cancer. 2012 Jul 30. doi: 10.1002/cncr.27503. [Epub ahead of print] [PUBMED]
- 8Ilic D, Djulbegovic M, Jung JH, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ. 2018;362:k3519. Published 2018 Sep 5. doi:10.1136/bmj.k3519 [PUBMED]
- 9Chou R, Croswell JM, Dana T, et al. Screening for prostate cancer: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;155(11):762–771. doi:10.7326/0003-4819-155-11-201112060-00375 [PUBMED]
- 10McDonald ML, Parsons JK. The Case for Tailored Prostate Cancer Screening: An NCCN Perspective. J Natl Compr Canc Netw. 2015;13(12):1576–1583. doi:10.6004/jnccn.2015.0183 [PUBMED]
- 11Bjurlin, Marc A, and Stacy Loeb. “PSA Velocity in Risk Stratification of Prostate Cancer.” Reviews in urology vol. 15,4 (2013): 204-6. [PUBMED]