- The topics covered on this page include:
- Mammaprint®- A test to determine the likelihood that breast cancer will recur
- Oncotype DX® (breast cancer) - A test to determine which chemotherapy drugs are likely to be effective and the likelihood that the cancer will recur within 10 years.
- Oncotype DX® (colon cancer) - A test to determine the likelihood the cancer will recur. Used only for stage 2 colon cancer.
- P
Cancer is a disease that results from genetic changes (changes to the patients' DNA). Understanding the genetic changes that take place in cancer allow us understand the disease. As technology improves, it is easier (and less expensive) to idenfity the exact changes that have occured in any particular cancer patient. The development of new, targeted drugs means that knowing the exact genetic changes in any given patient is increasingly important in determining the right treatments for that individual. The tests currently available are designed to predict how likely a particular cancer is to respond to a chemotherapy drug or how likely the cancer is to come back (recur) after it has been removed.
Diagnostic tests are able to examine:
1. The presence/absence/amount of a specific protein.
Examples of this include blood tests (CEA, CA-125) and tests performed on tumor samples obtained by biopsies (ER, HER2/neu). These types of tests have been available for many years and are routinely performed on patient samples.
2. The activity (expression) of a gene or set of genes.
The 'expression' of a gene refers to its transcription from DNA to RNA. All genes are not expressed equally in every cell; some may not be expressed at all. Cells express only the genes they require at any given time to survive and perform necessary functions. Altered gene expression is part of the process by which normal cells become cancerous. Extensive research is being performed to identify ways to monitor gene expression more effectively. Knowledge of which genes are aberrantly expressed in cancerous tissues has great potential to benefit cancer patients and even to help in cancer prevention.
Testing for gene expression by older methods only allows monitoring of a few genes at a time. GeneChip® analysis allows researcher to monitor hundreds to thousands of genes simultaneously. By monitoring many genes at once, sets of genes can be recognized as having altered expression. GeneChip® analysis employs a small quartz chip to which known fragments of DNA are attached. The DNA fragments on the chip may represent all of the genes in a cell.
The technology utilizes RNA purified from cells. Using an enzymatic process, the RNA is copied into DNA (cDNA) and the cDNA is labeled with a fluorescent (colored)dye. A control sample of normal tissue is treated in a similar fashion, with a dye of a different color. Aliquots of both samples are added to the array on the chip, to allow complementary nucleotides in the nucleic acid strands to pair with each other. RNA from genes that are expressed at a high level in cancer cells will be present in the samples at higher levels. The cDNA from these genes will bind to the gene chip in larger numbers and will exhibit more fluorescence. Levels of fluorescence for the genes on the chip are compared to determine which genes are expressed at higher and lower levels in cancerous tissues. Using mathematical approaches, sets of genes that have changes in their expression organized into groups.
Collectively, the display is referred to as an expression pattern. It is hoped that these expression patterns can be used to:
- Create diagnostic tests that are less invasive or are better indicators in early stage disease.
- Help identify new targets for treatment.
- Provide a means to better classify cancers.
- Allow for the generation of personalized treatment plans.
Several different companies are involved in creating/exploiting this technology. Affymetrix was one of the first companies involved. Learn more about GeneChip® technology from Affymetrix.
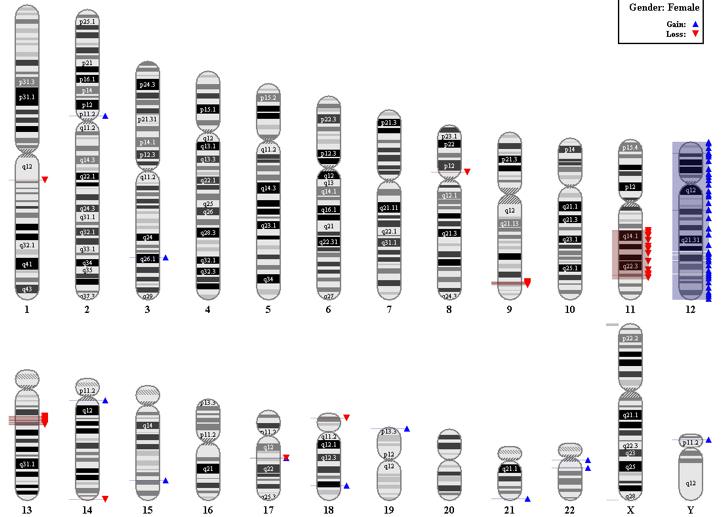
3. Genetic abnormalities (mutations) and epigenetic changes:
Mutations are changes to the DNA that alter the sequence of bases (A, C, G, and T) in our genes. Changes to critical genes are known to occur in cancer and new tests are being designed to identify these changes in tumor samples. The exact combination of changes found may make it likely that a particular treatment will work or is unlikely to have an impact. Epigenetic changes are also modifications to the bases, but they don't change the actual sequence. It is more like switching a lowercase a to uppercase A. The result is still altered gene activity and these changes are frequently seen in cancer.
New research has shown that it is possible to sequence the entire genome of cancer patients to find all possible changes in a timely and cost effective manner. This opens the door to many new diagnostic tests.
Learn more about mutations. Learn more about epigenetic changes.
Several molecular tests are available both inside and outside of the hospital setting. These 'direct to consumer' or DTC tests do not always need approval by the Food and Drug Administration (FDA) and caution is always urged for any tests of this nature. As in any medical test, it is important to understand how to interpret the results. As an example - if the results indicate that a persons' risk for developing a particular cancer is increased by 100% ( a two-fold increase) - what does that mean? If only one in 10,000 people without the identified risk get the disease, then the result means that the new risk is still only 1 in 5000 people. It is important to understand 'relative risk' (2 fold increase) vs 'absolute risk' (1 in 5000).
Available Molecular Diagnostic Tests
Mammaprint®
The MammaPrint® test was developed by Agendia. The test is designed to provide breast cancer patients with additional information about the likelihood that their cancer will return (recur).
What the test does. The MammaPrint® test requires a sample of the tumor. The tumor tissue is examined to determine the activity levels (transcription levels) for 70 different genes that have previously been shown to be involved in the spread (metastasis) of breast cancer. Based on which genes are active, and their levels of activity, the test is able to predict how likely any particular cancer is to return after surgery.
Which patients should consider MammaPrint®? The test has been shown to be useful for women with early stage invasive breast cancer (stage 1 or 2), whose cancer has not been shown to have spread to their lymph nodes (node negative). The presence or absence of the estrogen receptor (ER) does not influence the test.
What are the results of the MammaPrint® test? The test has only two possible outcomes. Results are classified as either 'low risk' or 'high risk'. For patients whose tumors measure as 'high risk', the tumor has a 29% chance of returning within 10 years if the patient does not take ANY additional treatment.
For patients whose tumors measure as 'low risk', the tumor has a 10% chance of returning within 10 years if the patient does not take ANY additional treatment.
The results are used in combination with all of the other available information about the patient to help decide what additional treatments the patient should take (i.e. hormonal treatments and/or chemotherapy).1 2
The MammaPrint test was the first genetic test of its kind to be approved by the US Food and Drug Administration (FDA).3
Oncotype DX® (breast cancer)
Oncotype DX® for Breast Cancer
What the test does.
Oncotype DX® for breast cancer was developed by Genomic Health.4 The purpose of the test is to predict how likely breast cancer is to return (recur) within 10 years. The test is performed on a sample of tumor tissue collected during biopsy/lumpectomy/mastectomy. The test measures the activity of 16 genes that have been shown to be important in the growth and/or spread of breast cancer and the activity of 5 reference (unrelated) genes.
Which patients should consider Oncotype DX®:
Women of any age who were recently diagnosed with Stage I or II lymph node negative, estrogen receptor positive (ER+) breast cancer can consider testing in order to help determine whether chemotherapy would be of benefit to them.
Post-menopausal women recently diagnoses with lymph node positive cancer may also be able to use the test.
What are results of Oncotype DX®
The main result of the testing is a Recurrence Score®. The score is reported on a scale of 0-100, based on the activity levels of the 21 genes. The score is used to make two different predictions.
- What is the likelihood that the breast cancer will return at a distant site (i.e. lungs, liver, etc.) within 10 years if the patient takes only tamoxifen.
- What would the benefit be to the patient of adding chemotherapy to their treatment?
The results contain graphs that include the patient’s result. Any patient who is not confident in their ability to interpret the results should discuss them with a qualified individual. The predictions are based on clinical trials using OncoTypeDX®. All patients in the studies used to validate the test took tamoxifen, a hormonal breast cancer treatment.5 6 7
In general, patients with low Recurrence Scores® are less likely to have their cancer recur and less likely to benefit from the addition of chemotherapy to their treatment. In the studies done to prove the accuracy of the Oncotype DX® test, the chemotherapy drugs used were methotrexate and fluorouracil with or without cyclophosphamide.
The report also includes detailed information on the results for three of the 21 genes examined in the test. They are 1) the estrogen receptor (ER), 2) the progesterone receptor (PR), and 3) the epidermal growth factor receptor 2 (HER2). The ER and HER2 genes are specifically listed out because the levels of the protein products of these genes are linked to responses to hormonal and antibody-based treatments for breast cancer.
The cost of this test is covered by many insurance companies and is recommended for specific types of patients by the American Society for Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN).8
Oncotype DX® (colon cancer)
What is the Oncotype DX® test for colon cancer?
In cancer, some genes are too active, and some are turned down too much. This test was develped by Genomic Health and is designed to look at the activity of 12 genes. Seven of the genes are known to be involved in colon cancer growth and/or spread. The other five allow the lab to make sure the test is working properly. The test is performed on colon cancer tissue removed during surgery. The purpose of the test is to make predictions about how likely the cancer is to return (recur) after it is removed surgically. If the cancer is likely to return, the patient may choose to take chemotherapy.9
10
The test has been validated by clinical studies of colon cancer patients but is still under review and has not yet been adopted by the major clinical cancer organizations as part of standard cancer treatment. At least one publications concludes that additional testing is necessary to confirm the usefulness of the test to patients.10 11
What patients may choose to get the Oncotype DX® test?
The test is for patients who have confirmed stage 2 colon cancer.
What are the results of the test?
The end result of the testing is a 'Recurrence Score®', a number between 0 and 100. The higher the number, the more likely the cancer is to recur in the the three years following the surgery. The report provides graphs and printed results.9
Note that this test has not been cleared by the FDA and it is not currently included in standard colon cancer staging/diagnosis guides (ASCO, NCCN).
- 1Bueno-de-Mesquita JM, Linn SC, Keijzer R, Wesseling J, Nuyten DS, van Krimpen C, Meijers C, de Graaf PW, Bos MM, Hart AA, Rutgers EJ, Peterse JL, Halfwerk H, de Groot R, Pronk A, Floore AN, Glas AM, Van't Veer LJ, van de Vijver MJ. Validation of 70-gene prognosis signature in node-negative breast cancer. Breast Cancer Res Treat. 2009 Oct;117(3):483-95. Epub 2008 Sep 26. [PUBMED]
- 2Mook S, Schmidt MK, Weigelt B, Kreike B, Eekhout I, van de Vijver MJ, Glas AM, Floore A, Rutgers EJ, van 't Veer LJ. The 70-gene prognosis signature predicts early metastasis in breast cancer patients between 55 and 70 years of age. Ann Oncol. 2010 Apr;21(4):717-22. Epub 2009 Oct 13. [http://annonc.oxfordjournals.org/content/21/4/717.abstract] [PUBMED]
- 3https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/denovo.cfm?ID=DEN070009
- 4Oncotype DX® for breast cancer. Genomic Health Website. [http://www.oncotypedx.com/en-US/Breast.aspx]
- 5Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer.N Engl J Med. 2004 Dec 30;351(27):2817-26. Epub 2004 Dec 10. [http://www.nejm.org/doi/full/10.1056/NEJMoa041588] [PUBMED]
- 6Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, Ravdin P, Bugarini R, Baehner FL, Davidson NE, Sledge GW, Winer EP, Hudis C, Ingle JN, Perez EA, Pritchard KI, Shepherd L, Gralow JR, Yoshizawa C, Allred DC, Osborne CK, Hayes DF; Breast Cancer Intergroup of North America. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010 Jan;11(1):55-65. Epub 2009 Dec 10. [http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045%2809%2970314-6/abstract] [PUBMED]
- 7Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, Costantino JP, Geyer CE Jr, Wickerham DL, Wolmark N. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006 Aug 10;24(23):3726-34. Epub 2006 May 23. [http://jco.ascopubs.org/content/24/23/3726.abstract] [PUBMED]
- 8Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, Somerfield MR, Hayes DF, Bast RC Jr; American Society of Clinical Oncology. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol. 2007 Nov 20;25(33):5287-312. Epub 2007 Oct 22. [http://jco.ascopubs.org/content/25/33/5287.abstract] [PUBMED]
- 9 a b Oncotype DX® website (Genomic Health). Accessed 12-08-2011 [http://www.oncotypedx.com/en-US/Colon.aspx]
- 10 a b Gray RG, Quirke P, Handley K, Lopatin M, Magill L, Baehner FL, Beaumont C, Clark-Langone KM, Yoshizawa CN, Lee M, Watson D, Shak S, Kerr DJ. Validation Study of a Quantitative Multigene Reverse Transcriptase-Polymerase Chain Reaction Assay for Assessment of Recurrence Risk in Patients With Stage II Colon Cancer. J Clin Oncol. 2011 Nov 7. [Epub ahead of print] [http://jco.ascopubs.org/content/early/2011/11/03/JCO.2010.32.8732.long] [PUBMED]
- 11Webber EM, Lin JS, Evelyn P Whitlock. Oncotype DX tumor gene expression profiling in stage II colon cancer. Application: prognostic, risk prediction. PLoS Curr. 2010 Sep 2;2. pii: RRN1177. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2940137/] [PUBMED]