Malignancies of the skin are the most commonly diagnosed cancer type worldwide.1 The foremost cause of skin cancer remains UV radiation from sunlight. However, this disease, classically seen in older adults, is becoming increasingly common in younger populations due to tanning beds and exposure to other cancer-causing elements. Skin cancer may be classified as either non-melanoma skin cancer (cancer types include squamous cell carcinoma and basal cell carcinoma) or melanoma. The most common type of skin cancer is basal cell carcinoma. Melanoma which accounts for only 4% of skin cancer is responsible for 80% of skin cancer deaths.1
The incidence of skin cancer is very high. It is the most common of all cancers. However, the exact numbers are not known because cases of basal cell and squamous cell skin cancers aren't always reported to cancer registries, partly because of their low lethality and very high curability rates. In 2006 it is estimated that over 2 million people were treated for non-melanoma skin cancers.2 In 2023, the American Cancer Society estimates that there will be 97,10 new cases of melanoma and 7,320 new cases of other non-epithelial skin cancer, with 7,990 melanoma-related deaths and 4,480 deaths from other non-epithelial skin cancers.3
Young men DO get cancer. View the clip and then watch an interview with Philip Groom, a skin cancer survivor diagnosed when he was 16 years old.
Please visit the following sections to learn more about skin cancer.
- Anatomy of the Skin.
- Types of Skin Cancer
- Risk Factors (general)
- Risk Factors (melanoma)
- Symptoms and Detection
- Pathology Report and Staging
- Tumor Biology
- Treatment
- Skin Cancer Resources
- Section Summary
Interactive Games from CQ:
Skin Cancer Education:
CancerQuest, with help from the Melanoma Group at the Winship Cancer Institute of Emory University, has developed a skin cancer curriculum. The curriculum is available free for educational (non-profit) uses. View/Download the curriculum.
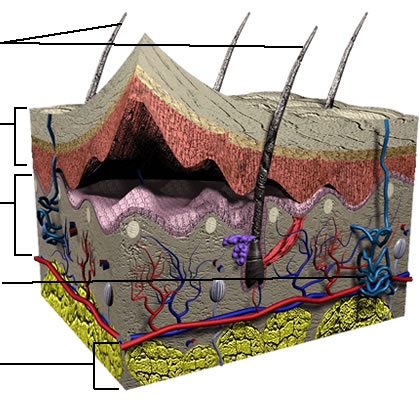
Anatomy Of The Skin
The skin is one of the largest organs of the body4 and is responsible for providing protection to the other systems of the body. Skin prevents water loss and dehydration, shields the internal organs in the event of injury, regulates body temperature, senses outside stimuli such as touch as well as heat and cold, and serves as a barrier to infection.5 As seen below, the skin is made up of three layers: the outer epidermis, the dermis and the deep subcutis layer. Other important elements of the skin include: hair follicles, sweat glands and nerve endings. Hair follicles protrude into the dermis layer and help regulate body temperature. Microscopic pores on the surface of the skin are connected to sweat glands which also help maintain homeostasis.

The pigments that color skin are produced by cells called melanocytes. Melanocytes, located in the epidermis (specifically in the stratum basale as seen in the diagram above), synthesize melanin which determines the color of the skin, hair and eyes.6 An individual's skin color is determined by their genes and their environment (primarily sun exposure). Our skin can change color in reaction to sun exposure. This is called the "tanning response." When skin absorbs UV radiation, melanin is produced and transferred to keratinocytes altering (darkening) the color of the skin.7Melanin in the skin absorbs and scatters UV radiation entering the body and helps protect the skin from adverse reactions to radiation, such as DNA damage (gene mutation). Viewed this way, the "tanning response" is really a defensive reaction by the body to the presence of damaging radiation.6
Types Of
Skin cancer may be divided into two types: non-melanoma and melanoma.
Non-melanoma Skin Cancer
There are two major sub-types of non-melanoma skin cancer:
Basal Cell Carcinoma- The most commonly diagnosed skin cancer. Tumors often develop on regions of the body that receive regular sun exposure such as the face and hands. Due to its slow growth rate, basal cell carcinoma rarely spreads and is usually treatable.8 A common form of basal cell carcinoma is nodular basal cell. Lesions appear as pearly nodules in various colors including brown, black and blue.9
Some examples:
![]()
Images used courtesy of the Skin Cancer Foundation
Squamous Cell Carcinoma- Appears on body parts that experience increased levels of sun exposure such as the face, lips and back.8 This cancer is more likely to spread than basal cell carcinoma. The cancerous lesions have numerous forms. They may be rough, scaly, lumpy or flat. Blood vessels may appear at the edge of a lesion causing it to bleed easily.8
Some examples:
![]()
Images used courtesy of the Skin Cancer Foundation.
Melanoma Skin Cancer
Melanoma is a cancerous growth of melanocytes and most frequently develops in the skin.1 Melanoma may also develop in other parts of the body that contain melanocytes including the meninges, the digestive tract, the eyes and lymph nodes. The following descriptions are limited to melanoma of the skin.
There are several types of melanoma that can be categorized based on their appearance, either with the naked eye or microscopically:
- Superficial spreading: The most frequently observed melanoma. This form may develop in any region of the skin. Lesions are usually raised around the edges and a brown color with hints of pink, white, gray and blue.
- Nodular type lesions: Also arise on all regions of the body and are typically black or brown in color.
- Acral lentiginous lesions: Characterized by flat, brown or black tumors that often develop on the hands and feet.
- Lentigo maligna melanoma: Develop on an individual's face. Distinguished by its irregular border and tan to brown color.10
Some examples of melanomas that demonstrate the irregular shapes and colors often encountered:

Images used courtesy of the Skin Cancer Foundation.
Risk Factors
The following risk factors that influence one's risk of developing skin cancer are discussed below:
- Ultraviolet Radiation1
- Skin Color10
- Sun Sensitivity
- Immunosuppression
- Prior Diagnosis9
- Family History
- Radiation Therapy11
- Smoking8
- Chemical Exposure8
- Drugs used to treat other conditions12
- Injury8
- Geographic Location
- Infection with HPV?13
Ultraviolet Radiation
Overexposure to ultraviolet (UV) radiation may cause genetic changes (mutations) in skin cells. The genetic changes cause the affected cells to alter their behavior and may result in cancer.1 Sources of UV radiation include the sun and tanning beds. Ultraviolet radiation also induces the production of very reactive chemicals, oxidants, in affected cells.1 Oxidants cause some of the changes associated with aging and increase one's risk of developing cancer.
Tanning beds are a dangerous source of UV radiation. They have been associated with all major types of skin cancer - basal cell carcinoma, squamous cell carcinoma, and melanoma. Tanning beds have been designated as a cancer causing agent by the World Health Organization.14, 15 The use of a tanning bed increases a person's risk of developing melanoma, regardless of whether the person gets sunburned.16
Below is a diagram showing the radiation from the sun and which parts make it to the surface of the earth. This graphic is interactive, so click on the different boxes to see the penetration of different types of light (including UV) and to see the layers of the atmosphere.
Skin Color & Sun Sensitivity
Fair skin is more susceptible to ultraviolet radiation damage.10 Caucasians, specifically individuals with freckles, light eyes and/or red hair, are at higher risk of skin damage that may lead to skin cancer.10
Immunosuppression
Immunosuppressants weaken the action and efficacy of the immune system and hinder its ability to fight foreign invasion. 1Immunosuppression may support the development of cancer. A weakened immune system is less able to eliminate cells that have suffered mutations and have the potential to develop into cancer cells. In addition, immunosuppressant therapies may have direct cancer causing consequences.17
Drugs used to treat other illnesses
Thiopurines, a class of drugs used to treat inflammatory diseases (i.e. Crohn's disease and inflammatory bowel syndrome) and some forms of cancer, have been shown to increase the risk for the development of non-melanoma skin cancers.12
Personal History
Survivors of skin cancer have an increased risk of developing a secondary cancer.1 The greatest risk for relapse is within the first five years following treatment. This heightened risk may be a result of a biological predisposition, previous exposure to skin cancer risks or a consequence of the initial cancer treatment itself.
Radiation Therapy
Radiation therapy is often used in the medical field in the treatment of primary cancers. Irradiation of primary tumors often exposes normal skin to increased levels of radiation and may lead to the development of secondary cancers, including skin cancer. The cancers arise due to mutations within skin cells caused by high doses of radiation.11
Chemical Exposure
Chronic exposure to arsenic, industrial tar and paraffin may increase one's risk of developing skin cancer.8
Serious injury
In some instances, skin cancer development is associated with serious injury or inflammation.8 Malignant growths that arise at sites of previous serious/chronic wounds such as burns and pressure ulcers are termed Marjolin ulcers.18
Risk Factors For Melanoma
Risk factors specific to melanoma:
Watch the video below to learn about some great skin cancer prevention tips. Watch the full interview with Dr. Suephy Chen.
Sun exposure:
Sun exposure increases one's risk of skin cancer. Individuals are inevitably exposed to sunlight, or ultraviolet radiation, during their daily activities. However, certain outdoor behaviors elevate an individual's likelihood of developing cancer. Infrequent, but intense exposure to sunlight during childhood increases one's risk of developing melanoma. 1Melanoma is often observed in areas of the body that receive infrequent but intense sun exposure such as the neck and the back of the legs.19
Also, it is important to note that cutaneous melanoma may occur in regions of the body typically shielded from sunlight such as the groin and bottom of the feet.
Family History
Individuals who have first degree relatives, including parents, siblings or children, diagnosed with melanoma have an 8 to 12 fold increased chance of developing melanoma. 10This increased risk is likely due to a biological predisposition to cancer development.
Melanocytic Nevi
The medical term for a marking on the skin, such as a mole or birthmark, is "nevus" (plural-nevi). Most melanocytic nevi develop during childhood and adolescence as a result of sunburn and sun exposure. The presence of melanocytic nevi is associated with an increased risk of developing melanoma.10
Symptoms And Detection
The American Academy of Dermatology and the American Cancer Society recommend that individuals perform monthly self-examinations.10 It is important to keep the ABCDE's (Asymmetry, Border, Color, Diameter, Evolution) of melanoma in mind.:
- Asymmetry: melanomas tend to be asymmetrical while benign lesions are more rounded and symmetric.
- Borders: Benign lesions are usually regular and flush with the skin while melanomas may have irregular and/or raised borders.
- Color: Melanomas may be tan, black or brown and often include regions of red, white and blue.
- Diameter: In general, melanomas are larger than 6 mm in diameter.
- Evolution: Changes in physical appearance of melanocytic growths are often observed over time and skin marking should be monitored for changes. Because the changes may be gradual, it is a good idea to photograph any suspicious marks, including a ruler or coin for size comparison. This allows for a direct comparison of images taken at different times.
Although the ABCDE guidelines assist with a valuable screening tool, it is important to see a physician regularly and especially if one finds a suspicious or irregular skin marking/growth or witnesses a change in an existing skin marking/growth.10
Asymmetry: | Border: |
Color: | Diameter: |
Images used courtesy of the Skin Cancer Foundation
An imaging system, MelaFind®, developed by Mela Sciences has been approved by the FDA to aid in the detection of melanoma. Learn more about MelaFind®.
Melanoma Staging
Pathology Report & Staging
Staging is a powerful tool for treatment plan development and risk assessment in individual patients. Staging also enables physicians to communicate with each other regarding patients' diseases and ensure equal standards of care for patients with similar disease states. 20The American Joint Committee on Cancer (AJCC) has developed a staging system for nonmelanoma and melanoma skin cancer.10
Staging of skin cancer is based on the TNM staging described in the CancerQuest section on Cancer Staging. Using this information, physicians may determine the stage of disease. The information below is specific for melanoma:
- Stage I: The disease is localized to a primary tumor site. The majority of diagnoses are during this stage.20
- Stage II: The disease is more developed, but remains localized to the original site.21
- Stage III: The disease has spread regionally; doctors often examine the number and location of invaded lymph nodes.20
- Stage IV: The melanoma has spread to distant organs.20
Several different approaches to staging of melanoma have been developed. Two criteria that have been used extensively include the categorization of melanomas according to their 'Clarks' levels' or 'Breslow thickness'. The Clark level is based on the layers of epidermis that the tumor has penetrated at the time of measurement. Breslow thickness measures the absolute distance of tumor penetration into the epidermis (measured in millimeters (mm)).
The Breslow tumor thickness evaluation system measures tumor thickness in mm from the top of the granular layer to the deepest tumor growth. The Breslow scale divides melanomas into four classes:
The "Clark levels of invasion" system, named after the developer, pathologist, Wallace Clark, was the first widely accepted method for staging of melanomas. It is considered a reliable staging system today, and tumors are classified as one of five categories. It is important to note that Clark levels are NOT the same as the stage of the disease.
- Level I Lesions: Melanoma restricted to the epidermis also known as an in situ melanoma.
- Level II Lesions: Melanoma crosses the epidermis and invades the papillary dermis. This may be referred to as the micro-invasive radial growth phase.
- Level III Lesions: The entry into the true tumor phase in which the tumor grows to fill the papillary dermis region. Such tumors have entered the vertical growth phase.
- Level IV Lesions: Tumor cells overcome barriers of the papillary dermis- reticular dermis barrier, invading the reticular dermis region.
- Level V Lesions: Tumor growth extends into the subcutaneous fat.22, 23
More advanced disease is generally associated with a decreased survival rate.20
View detailed staging information from the National Comprehensive Cancer Network (NCCN).
Tumor Biology
Genetic changes that occur in cancer cells include mutation of key regulatory genes, changes in protein products, and changes in the amount of product produced by genes (gene expression). As changes accumulate, cells become more abnormal and cancer may result. Details of genetic change associated with cancer can be found in the Mutation section. Some of the genetic elements that have been shown to be important in the development of skin cancer are discussed below:
MC1R Gene and α-melanocyte-stimulating hormone
The melanocortin receptor is responsible for binding alpha-melanocyte-stimulating hormone, the signal that initiates melanin production. Fair-skinned individuals have polymorphisms that reduce the affinity of MC1R resulting in decreased MC1R:alpha-MSH binding. As a result, melanin production is reduced, increasing the individual's risk of developing melanoma.24
CDKN2A
CDKN2A refers to a region of DNA coding for two tumor suppressor proteins:
Ink4A and Arf. Both proteins play a key role in cell cycle regulation. Reduced activity of these proteins has severe consequences on the ability of cells to regulate cell division. Mutations in CDKN2A result in reduced function of the p53 and RB tumor suppressor pathways.25
RAS Genes
RAS refers to a group of genes that are often mutated in cancer of many different types, melanoma included. The protein products are involved in transmitting signals through cells (also called "signal transduction") and are involved in numerous processes. Mutated RAS may increase malignant cell proliferation and reduce apoptosis. The pathways controlled by RAS have been found to be very frequently disrupted in melanoma cells.25
RAF Genes
The products of the three known RAF genes (RAF-1, ARAF and BRAF) function in the RAS pathway. The proteins are serine/threonine kinases and they function to transmit signals through the cell, influencing cell division. The BRAF gene product also seems to be involved in cell death (apoptosis). In one study, mutations in BRAF genes were observed in 66% of melanoma cell lines examined.25, 26
Bcl-2
This gene encodes a protein that regulates apoptosis. Mutations that increase the expression of Bcl-2 or enhance its function tend to reduce cell death and favor cancer development.25
Treatment
Both surgical and non-surgical approaches are used in the treatment of melanoma and non-melanoma skin cancers. 9Treatment of non-melanoma skin cancer is made more difficult by the high frequency of recurrence. 27For advanced melanoma, a highly successful treatment option for advanced disease has not yet to be identified.27
Surgical Treatment
Excision of a skin cancer lesion is a frequent treatment option. Excision may be curative for diseases that are in stages I or II (localized).10
- Learn about surgical treatment of cancer cells
- Watch an interview with skin cancer specialist Dr. Suephy Chen.
Non-surgical Treatment
Alternate treatment methods are preferred for patients whose health does not allow them to enter into surgery or for patients with cancerous lesions located in regions difficult to access surgically. Patients who undergo surgery may receive additional treatments. 27Examples of nonsurgical treatment options include:
Radiotherapy - the use of high energy waves, such as x-rays, to kill cancer cells.
- Photodynamic Therapy - a type of treatment in which an "inactive" medication is applied to the area of interest and then "activated" by exposure to specific wavelengths of light. In the case of skin cancer, the agent may be applied directly to the skin in the form of a liquid.28
Topical Drug Treatments: an ointment containing imiquimod (Aldara™) has been used to treat basal cell carcinoma, genital warts and actinic keratosis. Imiquimod is an immune response modifier that stimulates the immune system to eliminate cancer cells. View the package insert.
Learn about the immune response and cancer.
Learn more about Aldara™ from the manufacturer.Biological Treatments: biological treatments for melanoma include the use of interleukin 2 (IL-2).
Specific Inhibitors: Kinase inhibitors, including sorafenib (Nexavar®) are being evaluated for treatment of advanced melanoma.
Learn more about specific inhibitors.
Learn more about kinase inhibitors, including sorafenib (Nexavar®).
Learn more about Nexavar® from the manufacturer.
More Information
For information about how these and other cancer treatments work, refer to the Cancer Treatments section.
Information about clinical trials:
- General clinical trial information.
- Click here for information about clinical trials from the National Cancer Institute.
Click here for information about clinical trials from Georgia Clinical Trials Online.
Skin Cancer Resources
Risks for Skin Cancer
Melanoma Causes and Risk Factors (Skin Cancer Foundation)
Melanoma Education Foundation: Saving Lives Through Education
Risk Factors for Melanoma Skin Cancer (ACS)
Melanoma Risk Factors (Mayo Clinic)
Detection and Diagnosis of Skin Cancer
Winship Cancer Institute: Melanoma Diagnosis and Staging Make an Appointment
What You Need To Know About: Moles and Dysplastic Nevi (NCI)
What You Need to Know: Skin Cancer (NCI) (2010)
Basal and Squamous Cell Skin Cancer (ACS)
Why You Should Know About Melanoma (ACS)
Skin Cancer Treatments
American Academy of Dermatology: Skin Cancer Treatments
Skin Cancer Survivorship
Melanoma Patients' Information Page
Long Term Risks for Skin Cancer Survivors
Melanoma Side Effects of Treatment
International Skin Cancer Resources
Melanoma International Foundation
Skin Cancer (Cancer Research UK)
Skin Cancer (British Skin Foundation)
Canadian Skin Cancer Foundation
Melanoma (Canadian Cancer Society)
Save Your Skin Foundation (Canada)
Skin Cancer Council (Australia)
Section Summary
Introduction
- Malignancies of the skin are the most commonly diagnosed cancer type worldwide.
- Skin cancer is becoming increasingly common in younger populations.
Types of Skin Cancer
- Skin cancer can be divided into two types: melanoma and non-melanoma.
- Non-melanoma skin cancer has two major subtypes: basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
- Basal cell carcinoma is the most commonly diagnosed skin cancer.
- Melanoma is a cancerous growth of melanocytes and most frequently develops in the skin.
Risk Factors
- Overexposure to UV radiation causes genetic damage that can promote skin cancer development.
- Fair skin is more susceptible to ultraviolet radiation damage.
- Survivors of skin cancer have an increased risk of developing a second cancer.
- Exposure to certain chemicals and radiation increases the risk for skin cancer.
Symptoms and Detection
- The ABCDEs of skin cancer assist in early detection: Asymmetry, Border, Color, Diameter, Evolution
Pathology Report and Staging
- T/N/M staging is used in skin cancer. This system assigns a degree of severity based on size, lymph node involvement, and spread of the cancer.
- Other skin cancer staging systems consider the depth of penetration of the tumor into the epidermis.
Skin Cancer Tumor Biology
- Many genetic changes occur in cancer. Details can be found in the Mutation section.
- Genes that have been implicated in the development of skin cancer include MC1R, CDKN2A, RAS, RAF, and Bcl-2.
Treatment
- BCC and SCC are frequently removed via minor surgery.
- Early-stage melanomas can be surgically removed.
- Non-surgical treatments for skin cancer include: chemotherapy, radiotherapy, topical drug treatments, biological treatments and specific inhibitors.
Know The Flow: Melanoma
Know the Flow is an educational game for you to test your knowledge. To play:
- Drag the appropriate choices from the column on the right and place them in order in the boxes on the left. Note that you will only use five of the six choices to complete the game.
- When done, click on 'Check' to see how many you got correct.
- For incorrect answers, click on 'Description' to review information about the processes.
- To try again, choose 'Reset' and start over.
Please visit us on a larger screen to play this game.
Pick A Part: The Skin
Pick A Part is an interactive game for you to test your knowledge. To play:
- Drag the appropriate choices from the column on the bottom and place them in order in the boxes on the left. Note that you will only use five of the six choices to complete the game.
- When done, click on 'Check' to see how many you got correct.
- For incorrect answers, click on 'Description' to review information about the processes.
- To try again, choose 'Reset' and start over.
Please visit us on a larger screen to play this game.
For help please refer to the Anatomy of the Skin page.
Get It Together: The Skin
The jigsaw puzzle below is timed. See how quickly you can build the skin model shown below the puzzle!

Save The Surfer
Save the Surfer! Test your knowledge of skin cancer by answering before the sun's rays hit the surfer. If you need more time, put on some sunscreen!
- 1abcdefghij Miller AJ, Mihm MC Jr. "Melanoma." New England Journal of Medicine. 2006 Jul 6;355(1):51-65. [PUBMED]
- 2 Rogers, H., Weinstock, M., Harris, A., Hinckley, M., Feldman, S., Fleischer, A., & Coldiron, B. (2010). Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Archives of Dermatology, 146(3), 283–7. http://doi.org/10.1001/archdermatol.2010.19 (Original work published March 2010) [PUBMED]
- 3 American Cancer Society.Cancer Facts & Figures 2023. Atlanta: American Cancer Society. (2023). Retrieved from https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
- 4 Goldsmith LA. My organ is bigger than your organ. Arch Dermatol. 1990 Mar;126(3):301-2. [PUBMED]
- 5 Vander's Human Physiology: The Mechanisms of Body Function, 10/e. Eric P. Widmaier, Hershel Raff, Kevin T. Strang. 2006. McGraw-Hill Inc: New York, New York.
- 6ab Meredith P, Sarna T. "The physical and chemical properties of eumelanin." Pigment Cell Research. 2006 Dec; 19(6): 572-94. [PUBMED]
- 7 Tsatmali M, Ancans J, Thody AJ. "Melanocyte function and its control by melanocortin peptides." Journal of Histochemistry and Cytochemistry. 2002 Feb;50(2):125-33. [PUBMED]
- 8abcdefgh Holcomb SS. "Nonmelanoma skin cancer." Nursing. 2006 Jun;36(6):56-7. [PUBMED]
- 9abc Rubin AI, Chen EH, Ratner D. "Basal-cell carcinoma." New England Journal of Medicine. 2005 Nov 24;353(21):2262-9. [PUBMED]
- 10abcdefghijkl Rager EL, Bridgeford EP, Ollila DW. "Cutaneous melanoma: update on prevention, screening, diagnosis, and treatment." American Family Physician. 2005 Jul 15;72(2):269-76. [PUBMED]
- 11ab Ron E. "Cancer risks from medical radiation." Health Physics. 2003 Jul;85(1):47-59. [PUBMED]
- 12ab Singh H, Nugent Z, Demers AA, Bernstein CN. Increased risk of nonmelanoma skin cancers among individuals with inflammatory bowel disease. Gastroenterology. 2011 Nov;141(5):1612-20. Epub 2011 Jul 30. [http://www.gastrojournal.org/article/S0016-5085%2811%2901072-9/abstract] [PUBMED]
- 13 Iannacone MR, Gheit T, Waterboer T, Giuliano AR, Messina JL, Fenske NA, Cherpelis BS, Sondak VK, Roetzheim RG, Michael KM, Tommasino M, Pawlita M, Rollison DE. Case-control study of cutaneous human papillomaviruses in squamous cell carcinomas of the skin. Cancer Epidemiol Biomarkers Prev. 2012 Jun 15. [Epub ahead of print] [PUBMED]
- 14 Wehner MR, Shive ML, Chren MM, Han J, Qureshi AA, Linos E. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. BMJ. 2012 Oct 2;345:e5909. doi: . [PUBMED]
- 15 Mogensen M, Jemec GB. The potential carcinogenic risk of tanning beds: clinical guidelines and patient safety advice. Cancer Manag Res. 2010 Oct 28;2:277-82. [PUBMED]
- 16 Vogel, R., Ahmed, R., Nelson, H., Berwick, M., Weinstock, M., & Lazovich, D. (2014). Exposure to indoor tanning without burning and melanoma risk by sunburn history. Journal of the National Cancer Institute, 106(6), dju112. http://doi.org/10.1093/jnci/dju112 (Original work published June 2014) [PUBMED]
- 17 Lopez MM, Valenzuela JE, et al. "Long-term problems related to immunosuppression." Transplant Immunology. 2006 Dec;17(1):31-5. Epub 2006 Sep 26. [PUBMED]
- 18 Esther RJ, Lamps L, Schwartz HS. "Marjolin ulcers: secondary carcinomas in chronic wounds." Journal of the Southern Orthopaedic Association. 1999 Fall;8(3):181-7. [PUBMED]
- 19 Perlis C, Herlyn M. "Recent advances in melanoma biology". Oncologist. 2004; 9(2: 182-7. [PUBMED]
- 20abcde Petro A, Schwartz J, Johnson T. "Current melanoma staging." Clinical Dermatology. 2004 May-Jun;22(3):223-7. [PUBMED]
- 21 American Cancer Society. Cancer Facts & Figures 2010. Atlanta: American Cancer Society; 2010. [http://www.cancerquest.org/sites/default/files/assets/pdf/facts%26figures2010.pdf]
- 22ab Lomuto M, Calabrese P and A Giuliani. "Prognostic signs in melanoma: state of the art." 2004 18(3):291-300. [PUBMED]
- 23ab Elder DE, Gimotty PA, D Guerry. "Cutaneous melanoma: estimating survival and recurrence risk based on histopathologic features." 2005 Dermatol Ther. 18(5):369-85. [PUBMED]
- 24 van der Velden P, Lodewijk S, Bergman W, et al. "Melanocortin-1 Receptor Variant R151C Modifies Melanoma Risk in Dutch Families with Melanoma." American Journal of Human Genetetics. 69:774779, 2001. [PUBMED]
- 25abcd Haluska FG, Tsao H, et al. "Genetic alterations in signaling pathways in melanoma." Clinical Cancer Research. 2006 Apr 1;12(7 Pt 2):2301s-2307s. [PUBMED]
- 26 Davies H, Bignell GR, et al. "Mutations of the BRAF gene in human cancer." Nature. 2002 Jun 27;417(6892):949-54. [PUBMED]
- 27abc National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology, v2.2007. www.nccn.org
- 28 Fritsch C, Goerz G, Ruzicka T. "Photodynamic therapy in dermatology Archives of Dermatology." 1998 Feb;134(2):207-14. [PUBMED]