Prostate cancer is a common cancer affecting the lives of millions of men worldwide. The incidence of prostate cancer cases rose drastically in the early 1990s. This trend was probably due to advances in prostate screening and detection. However, incidence rates have fallen since 2006. On the other hand deaths due to prostate cancer have remained the same.
Prostate cancer is currently the most commonly diagnosed cancer for men other than skin cancer and ranks as the second leading cause of cancer death in men. In 2023, the American Cancer Society estimates 288,380 new cases will be diagnosed and 34,700 men will die of the disease in the United States.1
Below is a list of the information found within this section:
- Anatomy of the Prostate
- Prostate Cancer Risk Factors
- Symptoms
- Detection and Diagnosis
- Pathology Report and Staging
- Prostate Cancer Tumor Biology
- Treatment
- Prostate Cancer Resources
- Section Summary
- Additional Resources
Learn more about prostate cancer or make an appointment at the Winship Cancer Institute of Emory University.
Prostate: Anatomy
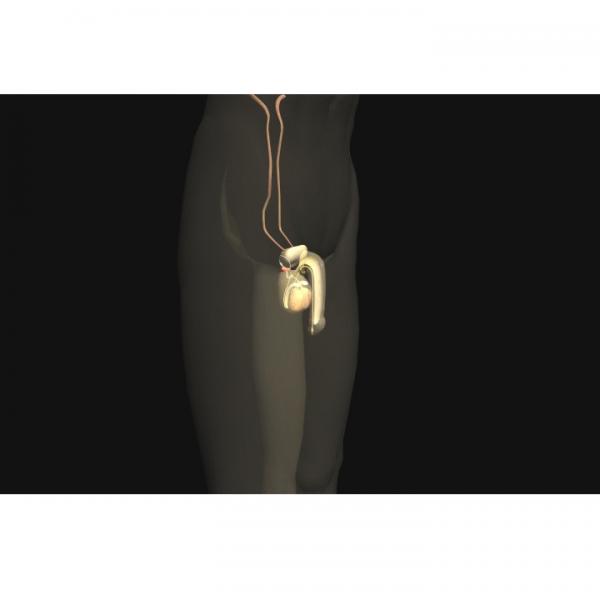
The prostate is a walnut-sized gland located in front of the rectum and just below the bladder. Although the prostate is made up of several cell types, almost all prostate cancers develop in the glandular cells.2 Cancer of gland cells is known as adenocarcinoma.
The glandular cells of the prostate normally make a fluid that is released into the urethra during ejaculation. This fluid forms part of the seminal fluid, which nourishes the sperm. Secretions from the prostate increase the pH of the semen and help to neutralize the acidity of the female vagina.
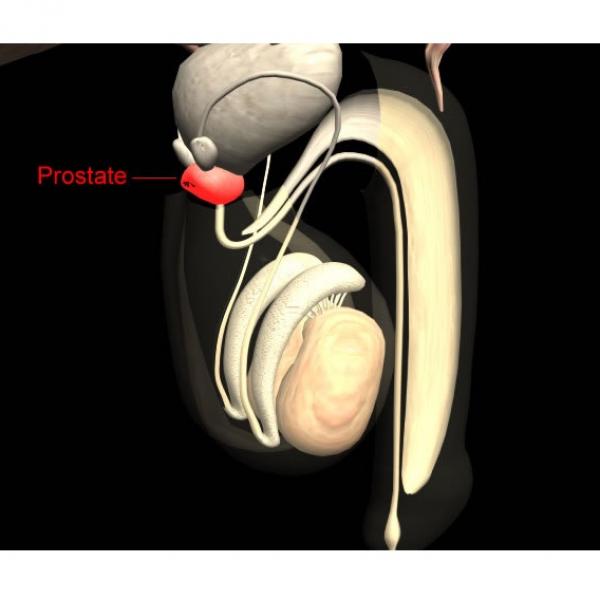
The prostate is surrounded by blood and lymphatic vessels:
- Blood vessels are part of the circulatory system. They supply oxygen and nutrients and remove waste from the cells of the prostate.
- Lymphatic vessels are part of a large network termed the lymphatic system. These vessels collect and carry fluid and cells from the tissues of the body. Smaller lymphatic vessels merge with larger ones, as streams merge into a river. Large vessels empty into grape-like clusters of lymphatic tissue called lymph nodes. The lymphatic vessels of the prostate carry lymphatic fluid to a mass of lymph nodes located in the pelvic region. Learn more about the lymphatic system here.
Risk Factors
Factors that may influence risk of developing prostate cancer include:
- Age
- Family History of Prostate Cancer
- Race
- Dietary Factors
- Infection with HPV/EBV
- Alcohol Consumption
The relative effects of these and other risk factors in any given case of cancer is variable and very difficult to determine with accuracy at this time.
Age
Risk of prostate cancer increases dramatically with age. Most patients are diagnosed with the disease over the age of 50.3 For more information about the relationship between age and cancer, refer to the Mutation section.
Family History of Prostate Cancer
It is possible to inherit dysfunctional genes that lead to the development of a familial form of a particular cancer type. Individuals with a family history of prostate cancer are therefore at an increased risk of developing the disease. The degree of risk depends upon the type of relative affected. For example, risk is higher if an immediate family member has been diagnosed with prostate cancer.4 The more closely related an individual is to someone with prostate cancer, the more likely they will share the same genes that predisposed the affected individual. Risk increases with the number of relatives affected.
Studies have linked several prostate cancer susceptibility genes to different locations within the genome.5 The mechanisms by which these genes lead to cancer, however, are still not well understood.
Race
African American men have the greatest incidence of prostate cancer in the United States. Cancer survival rates are greatly affected by the stage at which a cancer is detected. Compared to both European American and Hispanic men in the United States, African American males are also more likely to be diagnosed at a more advanced stage. Reasons for these differences among ethnic groups are still unclear. Such differences may be due to a combination of genetic, environmental, and/or social factors.6
Dietary Factors
It is very difficult to identify dietary items that cause a particular cancer. Studies indicate that many dietary factors may influence prostate cancer risk. It has been suggested that a diet rich in dairy and meat products may be associated with a higher risk, while a diet rich in fish and tomato-based products may be associated with a lower risk of prostate cancer.7 Studies suggest the accumulation of carcinogens that are generated when red meat is cooked at high temperatures may be a potential prostate cancer risk factor. 8
Infection with Human Papillomavirus and Epstein-Barr Virus
A 2012 Australian study examining both cancerous and healthy prostate tissue found an association between infection with HPV and EBV and an increased risk of prostate cancer. The role of the viruses in causing the cancer is not yet known.9
Alcohol Consumption
A 2016 review by BMC cancer links low, medium, high and higher alcohol intake with the occurrence of prostate cancer when compared with cancer development of those who abstain from alcohol consumption. The review incorporated information from over 300 studies to come to this conclusion, which helps validate the legitimacy of their claims. This information is important because now prostate cancer can be assessed in conjunction with other alcohol-related diseases.10
Symptoms
Symptoms
There are often no symptoms associated with early-stage prostate cancer. However, most cases of prostate cancer are diagnosed before symptoms develop through screening. The American Cancer Society lists the following symptoms associated with later-staged prostate cancer:11
- Inability to urinate
- Discontinuous or weak urine flow
- Difficulty in starting or stopping urine flow
- Frequent urination, especially at night
- Blood in urine
- Pain or burning with urination
- Continuous back, pelvis, or upper thigh pain
A physician should be consulted if they persist. It is important to note, however, that these symptoms may be caused by factors unrelated to prostate cancer.
Detection And Diagnosis
Prostate cancer is detected in several ways. The method used depends, in part, on the patient's preference and whether the cancer is causing any symptoms. Choosing any of the following will take you to the Diagnosis and Detection section. You can return to learn more about prostate cancer.
Prostate-Specific Antigen (PSA) Test
Pathology Report And Staging
The Pathology Report
If there is a suspicion that a patient may have prostate cancer, a sample of tissue (biopsy) may be taken for examination. After a biopsy is taken, the physician who performed the biopsy sends the specimen to a pathologist. The pathologist examines the specimens at both the macroscopic (visible with the naked eye) and microscopic (requiring magnification) levels and then sends a pathology report to the physician. The report contains information about the tissue's appearance, cellular makeup, and state of disease or normalcy. For more information about the pathology report, refer to the Diagnosis & Detection section.
Staging
Staging a cancer is a way of describing the extent of the disease. A common method of staging is called the T/N/M system, which assigns a degree of severity based on the size, location, and spread of cancer in the body. The most widely used grading system for prostate cancer, however, is the Gleason Grading System. This system assigns a number based on the aggressiveness of the prostate cancer. Details of the T/N/M system and Gleason Grading System can be found in the Diagnosis & Detection section.
Tumor Biology
Genetic changes that occur in cancer include mutation of key regulatory genes, changes in protein products, and changes in the amount of product produced by genes (gene expression). As changes accumulate, cells become more abnormal and cancer progresses. Details about these changes can be found in the Mutation section. Some of the genes that have been shown to be important in the development of prostate cancer are listed below and discussed on the following pages:
- Androgen Receptors
- PTEN Gene
- TP53 Gene
The Androgen Receptor
Male hormones such as testosterone are known as androgens. Androgen receptors (AR) are proteins found within the cell that help control growth and division. Once an androgen enters the cell and binds to an AR, the complex acts as a transcription factor, promoting cell growth. These receptors are important regulators of normal cell growth in the prostate.12
Several mutations can cause overexpression of the AR gene, resulting in unregulated prostate cell growth:
- The AR gene may be amplified. The resulting increase in expression of AR can lead to cell growth even in the presence of low levels of androgen.
- Mutations in the AR gene can alter the resulting protein and result in loss of binding specificity. Such mutations may result in the activation of the receptor by substances other than androgen.
- Mutations may cause the androgen receptor to be activated without the binding of any molecules.13
The correlation between AR expression and prostate cancer has led to the development of anti-androgens as a treatment option. For more information about the use of anti-androgen molecules in therapy, refer to the Cancer Treatments section.
Prostate cancers can develop the ability to grow without stimulation by an androgen. These cancers are called androgen-independent, or androgen-negative prostate cancers. Androgen-independent cancers are unlikely to respond to anti-androgen therapy.
PTEN
PTEN (phosphatase and tensin) homolog deleted on chromosome 10 is a tumor suppressor gene often mutated in prostate cancer. This gene plays an important role in several cellular pathways, including the control of prostate basal cell growth. Mouse models suggest that proliferation of these cells is an important step in the initiation and early progression of prostate cancer.14
For more information about tumor suppressors, refer to the Cancer Genes section.
p53
p53 is a tumor suppressor gene involved in DNA repair and the regulation of apoptosis. p53 mutations occur only in a small fraction of prostate cancers, and are usually associated with metastatic tumors.13
Treatment
The treatment of prostate cancer can be broken down into two categories: early stage and advanced stage. Early stage treatment involves tumors that are confined to the prostate. Advanced stage treatment involves tumors that have spread beyond the prostate gland. Treatment options are dependent upon size of tumor, location, physical condition of patient, and stage of cancer.
As our focus is on the biology of the cancers and their treatments, we do not give detailed treatment guidelines. Instead, we link to organizations in the U.S. that generate the treatment guidelines.
The National Comprehensive Cancer Network (NCCN) lists the following treatments for prostate cancer:
- Watchful waiting
- Radical prostatectomy
- Transurethral resection of the prostate (TURP)
- External beam radiation
- Internal radiation: brachytherapy
- Hormone therapy
- Removal of the testicles (orchiectomy)
- Antiandrogens
- Chemotherapy
Learn more about cancer treatments.
Information about clinical trials:
- General clinical trial information from CancerQuest
- Click here for information about clinical trials at the Winship Cancer Institute of Emory University
- Click here for information about clinical trials from the National Cancer Institute.
- Click here for information about clinical trials from Georgia Clinical Trials Online.
Prostate Cancer Resources
Risks for Prostate Cancer
Prostate Cancer Risk Factors (ACS)
What Are the Risk Factors for Prostate Cancer? (CDC)
Prostate Cancer Risks (Mayo Clinic)
Detection and Diagnosis of Prostate Cancer
Winship Cancer Institute: Prostate Cancer Diagnosis and Treatment Make an Appointment
What You Need to Know: Prostate Cancer (NCI)
Prostate Specific Antigen (NCI)
Selenium and Vitamin E Trials (NCI)
Prostate Cancer Treatments
Treatment Choices for Men With Early Prostate Cancer (NCI)
Prostate Cancer Research Institute: Treatment Options
Prostate Cancer Treatment (NCI)
Prostate Cancer Survivorship
US TOO International Support Group
National Alliance of State Prostate Cancer Coalitions
Long Term Risks for Prostate Cancer Survivors
Side Effects of Prostate Cancer (PCF)
Long Term Side Effects From Prostate Cancer Treatment (ACS)
Long Term Prostate Cancer Side Effects
International Prostate Cancer Resources
Prostate Cancer (Cancer Research UK)
Canadian Cancer Society: Prostate Cancer
Prostate Cancer Foundation of Australia
Cancer Council Australia: Prostate Cancer
Section Summary
Introduction
- Prostate cancer ranks as the second leading cause of cancer death in men.
- Almost all prostate cancers develop in the glandular cells.
Risk Factors
- Risk of prostate cancer increases dramatically with age. Most cases occur after the age of 50.
- The risk is higher if an immediate family member has been diagnosed with prostate cancer.
- In the US, African American men have the greatest incidence of prostate cancer.
- Dietary factors influence the risk of prostate cancer. Meat and dairy may heighten the risk whereas fish and tomato-based foods may lower the risk for prostate cancer.
Symptoms
- Advanced-stage prostate cancer patients experience a wide range of symptoms that may involve urine discoloration, pain with urination, weak urine flow, and others.
Detection and Diagnosis
- A prostate-specific antigen (PSA) test can be used to help detect prostate cancer, but it does not provide a definitive diagnosis.
Pathology Report and Staging
- A pathologist examines a tissue sample micro- and macroscopically in order to create a pathology report.
- Prostate cancer used the Gleason Grading System which assigns a number to the cancer based on its aggressiveness.
Prostate Cancer Tumor Biology
- Many genetic changes occur in cancer. Details can be found in the Mutation section.
- PTEN and TP53 are two of the genes involved in the development of prostate cancer.
- The androgen receptor protein binds androgens in the cell. This complex promotes cell growth and division. The presence or absence of this protein helps determine treatment options for the cancer.
Treatment
- A wide range of treatments exists for prostate cancer including chemotherapy, surgery, hormonal therapies and radiation.
- Foregoing treatment and carefully monitoring the prostate is an option in some cases.
Learn more about prostate cancer or make an appointment at the Winship Cancer Institute of Emory University.
- 1American Cancer Society. Cancer Facts & Figures 2016. Atlanta: American Cancer Society; 2016. [http://www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf]
- 2What Is Prostate Cancer? American Cancer Society. Accessed October 2010. [https://www.cancer.org/cancer/prostate-cancer/about.html]
- 3What Are The Risk Factors For Prostate Cancer? American Cancer Society. (Accessed October 2010) [http://www.cancer.org/Cancer/ProstateCancer/DetailedGuide/prostate-cancer-risk-factors]
- 4Cox B, Sneyd MJ, Paul C, Skegg DC. "Risk factors for prostate cancer: A national case-control study." Int J Cancer (2006) [epub ahead of print] [PUBMED]
- 5Verhage BA, Kiemeney LA. "Inherited predisposition to prostate cancer." European Journal of Epidemiology (2003); 18(11):1027-1036 [PUBMED]
- 6Consedine NS, Morgenstern AH, Kudadjie-Gyamfi E, Magai C, Neugut AI. "Prostate cancer screening behavior in men from seven ethnic groups: the fear factor." Cancer Epidemiol Biomarkers Prev (2006) Feb;15(2):228-37. [PUBMED]
- 7Wolk A. "Diet, lifestyle and risk of prostate cancer." Acta Oncologia (2005) 44:277-281 [PUBMED]
- 8Joshi AD, Corral R, Catsburg C, Lewinger JP, Koo J, John EM, Ingles SA, Stern MC. Red meat and poultry, cooking practices, genetic susceptibility and risk of prostate cancer: results from a multiethnic case-control study. Carcinogenesis. 2012 Nov;33(11):2108-18. doi: 10.1093/carcin/bgs242. Epub 2012 Jul 20. [PUBMED]
- 9Whitaker NJ, Glenn WK, Sahrudin A, Orde MM, Delprado W, Lawson JS. Human papillomavirus and Epstein Barr virus in prostate cancer: Koilocytes indicate potential oncogenic influences of human papillomavirus in prostate cancer. Prostate. 2012 Jul 31. doi: 10.1002/pros.22562. [Epub ahead of print] [PUBMED]
- 10http://bmccancer.biomedcentral.com/articles/10.1186/s12885-016-2891-z
- 11Cancer Facts and Figures 2013. American Cancer Society. [http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf]
- 12Mimeault Murielle, Batra SK. "Recent advances on multiple tumorigenic cascades involved in prostatic cancer progression and targeting therapies." Carcinogenesis (2006) 27(1):1-22 [PUBMED]
- 13 a b DeMarzo AM, Nelson WG, Isaacs WB, Epstein JI. "Pathological and Molecular Aspects of Prostate Cancer." Lancet (2003) 361(9361):955-964. [PUBMED]
- 14Wang S, Garcia A, Wu M, Lawson D, Witte O, Wu H. "Pten deletion leads to the expansion of a prostatic stem/progenitor cell subpopulation and tumor initiation." Proc Natls Acad Sci USA (2006); 103(5):1480-5 [PUBMED]