Introduction
Simply put, cancer is the result of unregulated cell division. Cancer cells divide when they are not supposed to, don't stop dividing when they are supposed to and don't die when they should. In the worst cases, the cancer cells leave the area in which they arose and travel to other parts of the body.
Cancer cells do not look or act like the normal cells from which they originate. It is reasonable, then, to ask 'Why do cancer cells behave so badly?'. It turns out the answers lie in the genes of the affected cells. In cancer cells, changes to key genes cause the cells to act abnormally. The changes are often the result of changes to the DNA (mutations) in the cells. Because there are many different things that are capable of causing mutation, there are an equally large number of causes of cancer.
The development of cancer takes place in a multi-step process. As the cells become more abnormal, they gain new capabilities, such as the ability to release growth factors and digestive enzymes. The cells continue to divide, impacting nearby normal cells, often reducing the function of the affected organ. Even abnormal cancer cells die sometimes and a tumor that is large enough to feel can take years to reach that size. Although not all cancers share exactly the same steps, there are some general features that are shared in the development of many types of cancer. Further information on the topics on this page can also be found in most introductory Biology textbooks, we recommend Campbell Biology, 11th edition.1
Below is a list of topics covered in this section:
Cancer Initiation, Promotion, and Progression
In the eighteenth century, London physician Percival Pott made the first link between cancer and environmental agents when he noted a high incidence of scrotal cancer among chimney sweeps. He hypothesized that it was caused by exposure to coals and tars. Out of this observation grew the two-stage model of cancer development by 1) initiators and 2) promoters. In the years since Pott's observations a wide range of chemicals, radiation sources, viruses and bacteria have been implicated in the development of cancer. 2
The initial experimental studies of carcinogenesis were conducted in animals. Chemicals able to react with DNA and non-reactive compounds were both tested for their ability to cause cancer. The model used was mouse skin carcinogenesis. In this system researchers painted test chemicals on the skin and observed the growth of tumors. Researchers found that application of a DNA reactive substance only resulted in tumor formation when the animals were further treated with another non-reactive substance. A compound that reacts with DNA and somehow changes the genetic makeup of the cell is called a mutagen. The mutagens that predispose cells to develop tumors are called initiators and the non-reactive compounds that stimulate tumor development are called promoters. Approximately 70% of known mutagens are also carcinogens--cancer-causing compounds. 3 A compound that acts as both an initiator and a promoter is referred to as a 'complete carcinogen' because tumor development can occur without the application of another compound. 4
Initiation
Initiation is the first step in the two-stage model of cancer development. Initiators, if not already reactive with DNA, are altered (frequently they are made electrophilic) via drug-metabolizing enzymes in the body and are then able to cause changes in DNA (mutations). 4 Since many initiators must be metabolized before becoming active, initiators are often specific to particular tissue types or species. 5 The effects of initiators are irreversible; once a particular cell has been affected by an initiator it is susceptible to promotion until its death. Since initiation is the result of permanent genetic change, any daughter cells produced from the division of the mutated cell will also carry the mutation. 4 In studies of mouse skin carcinogenesis, a linear relationship has been observed between the dose of initiator and the quantity of tumors that can be produced, thus any exposure to the initiator increases risk and this risk increases indefinitely with higher levels of exposure. 5
Promotion
Once a cell has been mutated by an initiator, it is susceptible to the effects of promoters. These compounds promote the proliferation of the cell, giving rise to a large number of daughter cells containing the mutation created by the initiator. 3 Promoters have no effect when the organism in question has not been previously treated with an initiator. 5
Unlike initiators, promoters do not covalently bind to DNA or macromolecules within the cell. Many bind to receptors on the cell surface in order to affect intracellular pathways that lead to increased cell proliferation. 4 There are two general categories of promoters: specific promoters that interact with receptors on or in target cells of defined tissues and nonspecific promoters that alter gene expression without the presence of a known receptor. Promoters are often specific for a particular tissue or species due to their interaction with receptors that are present in different amounts in different tissue types.
While the risk of tumor growth with promoter application is dose-dependent, there is both a threshold and a maximum effect of promoters. Very low doses of promoters will not lead to tumor development and extremely high doses will not produce more risk than moderate levels of exposure. 5
Progression
In mice, repeated promoter applications on initiator-exposed skin produces benign papillomas. Most of these papillomas regress after treatment is stopped, but some progress to cancer. The frequency of progression suggests that the papillomas that progress to cancer have acquired an additional, spontaneous, mutation. 6 The term progression, coined by Leslie Foulds, refers to the stepwise transformation of a benign tumor to a neoplasm and to malignancy. Progression is associated with a karyotypic change since virtually all tumors that advance are aneuploid (have the wrong number of chromosomes). This karyotypic change is coupled with an increased growth rate, invasiveness, metastasis and an alteration in biochemistry and morphology. 5
Stages of Tumor Development
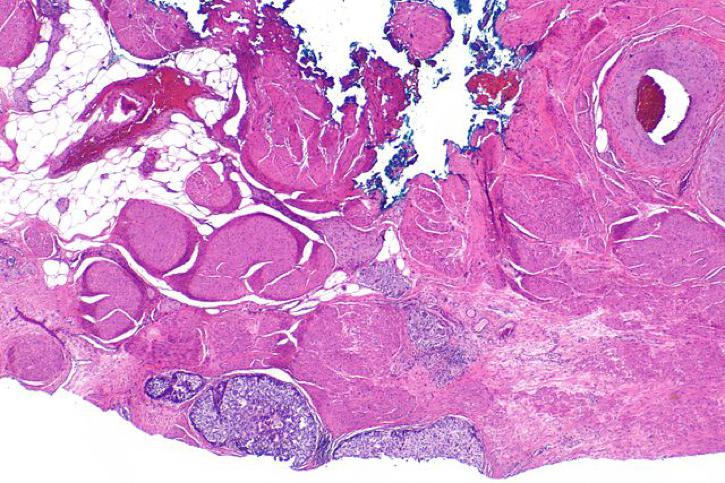
The growth of a tumor from a single genetically altered cell is a stepwise progression. The process described below is applicable for a solid tumor such as a carcinoma or a sarcoma. Blood cell tumors go through a similar process but since the cells float freely, they are not limited to one location in the body.
Hyperplasia- The altered cell divides in an uncontrolled manner leading to an excess of cells in that region of the tissue. The cells have a normal appearance but there are too many of them!
Dysplasia- Additional genetic changes in the hyperplastic cells lead to increasingly abnormal growth. The cells and the tissue no longer look normal. The cells and the tissue may become disorganized.
Carcinoma in situ- Additional changes make the cells and tissues appear even more abnormal. The cells are now spread over a larger area and the region of the tissue involved primarily contains altered cells. The cells often 'regress' or become more primitive in their capabilities. An example would be a liver cell that no longer makes liver-specific proteins. Cells of this type are said to be de-differentiated or anaplastic. A key facet of in situ growths is that the cells are contained within the initial location and have not yet crossed the basal lamina to invade other tissues. Cancers of this type are often totally curable by surgery since the abnormal cells are all in one location.
Tumors of this type have not yet invaded neighboring tissue. Based on information about patients with similar growths and microscopic examination, these growths are often considered to have the potential to become invasive and are treated as malignant growths.
Cancer (Malignant tumors)- These tumors have the ability to invade surrounding tissues and/or spread (metastasize) to areas outside the local tissue. These metastatic tumors are the most dangerous and account for a large percentage of cancer deaths. The next few sections will go into some detail on the changes and capabilities that allow cancer cells to form large tumors and to metastasize to other parts of the body.
Some tumors do not progress to the point where they invade distant tissues. Such tumors are said to be benign. Because they do not spread beyond their initial location, they are not considered to be cancerous. Benign tumors are less often lethal than malignant tumors, but they can still cause serious health problems. Large benign tumors can put pressure on organs and cause other problems. In the case of brain tumors, the limited space within the skull means that a large growth in the brain cavity can be fatal.
More information on this topic may be found in Chapters 13 and 14 of The Biology of Cancer by Robert A. Weinberg.
Cancer Stem Cells
What is a stem cell?
A stem cell is a special cell type that has both the ability to reproduce exact copies of itself (also called self-renewal) and the ability to change (differentiate) into one of the many specialized cell types in the body. Examples of specialized cells that arise from stem cells include nerves, muscles and the cells lining our digestive system.
In most parts of the body, stem cells are not very active. In some locations, including the gastrointestinal tract, stem cells divide and differentiate constantly to replace cells that are shed or die. Stem cells also play a role in healing damaged tissue.
Below is a video of the process by which stem cells can accomplish both self-renewal and differentiation. The process is called "asymmetric cell division," and it assures that stem cells are always available when needed.7
What is a cancer stem cell?
Cancer stem cells (CSCs) are thought to arise from normal stem cells. Sometimes, genetic changes or mutations damage normal stem cells, preventing them functioning properly. If this improper function includes uncontrolled reproduction, then the normal stem cell has the ability to form a tumor; it is now a cancer stem cell.
The existence of CSCs was predicted decades ago, but recent research has identified cancer stem cells in multiple cancer types, prompting extensive research in this field.7, 8
Where do cancer stem cells come from?
In theory, CSCs could be formed in more than one way. Mutations could occur in a differentiated cell (i.e. a skin cell) causing the cell to go backwards or 'devolve' into a cell with some stem cell abilities. Cancer stem cells could also be formed by the mutation of a normal stem cell that causes it to become cancerous. Cancer stem cells have been created in research laboratories from skin cells9 The researchers used a virus to activate specific pathways and give the target cell stem cell-like qualities. The research proves that a normal cell can become a stem cell with the right set of mutations.
The probability of any particular cell developing a set of mutations that leads to cancer is relatively low. The cells types that are affected by the majority of cancers, epithelial cells, have short lives and are even less likely to accumulate all the mutations they need. Normal stem cells, which are long-lived, are more likely to be around long enough to accumulate the necessary mutations and are a good possible source of cancer stem cells.7
What is the difference between the cancer stem cell hypothesis of the origin of cancer and traditional views on the origin of cancer?
The cancer stem cell hypothesis suggests that only a small portion of cells are capable of becoming cancerous. In other words, only a small population of cells in a tumor is responsible for the continuous, uncontrolled growth seen in cancer.
The traditional views on the origin of cancer predict that any cell is able to acquire mutations that lead to uncontrolled reproduction. Likewise, all of the cells in a tumor would be predicted to be able to divide endlessly.8
The Search for Cancer Stem Cells
What led to the search for cancer stem cells?
There are several reasons why many researchers find the cancer stem cell hypothesis appealing. Cancer stem cells provide one possible explanation for the frequent failure of cancer treatments, the large amount of cells needed to cause cancer growth in model organisms, and gaps in other theories of cancer development. A large challenge has been the identification and isolation of cancer stem cells. Researchers have identified some cell surface proteins (also called markers) found on cancer cells that have some important stem cell capabilities. These markers include CD44, CD133, and ALDH1.8
One of the pieces of evidence that favors the existence of cancer stem cells is the fact that when researchers look at tumors they appear to contain several differentiated cell types. The traditional theory on the development of cancer is able to explain this, but the large number of mutations necessary to create the mixture is unlikely. An illustration,- if tumors form from a single mutated cell the tumor would only contain cells of that type rather than cells of many types:
If multiple cells of different types in the same area have mutations this would lead to a tumor of mixed cell types:
Cancer stem cells have the ability to produce cells of many different types creating the mixture of cells found in a tumor:
The possibility of a stem cell becoming a cancer stem cell is, statistically, more likely to happen than multiple mutations in multiple cells in the same area in order to produce a tumor with multiple cell types.10, 8
Cancer Stem Cells and Treatment
What is the impact of CSCs on treatment?
Current treatments target cancer because the drugs act on cells that are actively dividing. Most of these drugs function by inducing the death (via apoptosis) of the cancer cells. Cancer stem cells carry mutations that lead to cancer, but they do not necessarily divide quickly. This relatively inactive state would allow them to avoid the effects of cancer treatments which would explain the all too frequent recurrences of cancers. CSCs also efficiently repair DNA damage and avoid apoptosis making them hard targets for today's drugs. This evasion of treatment could be likened to a weed in a garden. Cancer stem cells are like the roots of the weed and the majority of the tumor mass is the leaves and stem of the weed. Removing the visible part of the weed appears to kill it, but the roots underground soon sprout another stem and the weed lives on.11
Why is it difficult to target CSCs?
The problems encountered when clinicians treat cancer are also seen when purified CSCs are treated with anti-cancer drugs. Because normal stem cells and CSCs are very similar, it is difficult to kill CSCs and leave normal stem cells unharmed. Drug resistance is another major obstacle in treating both cancer and CSCs. Stem cells tend to have high levels of particular cellular pumps (i.e. the multiple drug resistance protein, MDR) that are able to eject cancer drugs from the cells making the drugs ineffective. Stem cells are also harder to kill than normal cells because they have an ability to block the signals that drugs like chemotherapy cause to lead to death (apoptosis). An excess of antiapoptotic proteins helps stem cells avoid the effects of cancer treatments.11
Can CSCs be targeted with treatment?
Cancer stem cells can cause problems with cancer treatments, but researchers are trying to come up with ways to target them. A potential cancer drug, napabucasin, has been found to target 'stemness.' According to two separate studies, a treatment combining napabucasin with chemotherapy was able to block STAT3 gene transcription in cancer stem cells.12 Napabucasin was shown to kill colorectal stem cells, block their renewal, and kill cancer cells13 Napabucasin could have serious side effects in humans, as it has been shown to cause bone loss in mice.14
It may also be possible to combine two non-lethal drug together in a way that will kill CSCs. An international collaboration looking into this found that combining an antibiotic (doxycycline) with vitamin C was effective at targeting CSC-like breast cancer cells.15
Learn more about MDR and drug resistance.
Learn more about cancer cell death (apoptosis).
Cancer Development Summary
Introduction
- All of our cells have similar structures and share a majority of their functions.
- Cancers may be categorized into five basic types based on the cell of origin:
- Carcinoma - epithelial cells
- Sarcoma - muscle, bone, cartilage, fat, or connective tissue
- Leukemia - blood cells or their precursors
- Lymphoma - bone marrow derived cells; cancer affects the lymphatic system
- Myeloma - specific blood cells; B lymphocytes (B-cells)
Stages of Tumor Progression
- Tumors typically progress is a stepwise fashion:
- Hyperplasia - cells divide too much but appear normal
- Dysplasia - the tumor cells and tissue appear abnormal
- Carcinoma in situ - tumor contains primarily altered cells and is growing larger; it has not left the site of origin
- Malignant Cancer - tumor has begun to invade nearby or distant tissues
- Benign tumors remain in their initial location and do not invade other tissues.
Initiators and Promoters
- Initiation is the first step in the two-stage model of cancer development.
- Initiators cause irreversible changes (mutations) to DNA that increase cancer risk.
- Promotion is the second step in the two-stage model of cancer development.
- Once a cell has been mutated by an initiator, it is susceptible to the effects of promoters.
- Promoters increase the proliferation of cells and there are two main types:
- Specific - interact with receptors on or in particular target cells.
- Nonspecific - alter gene expression without the presence of a known receptor
Carcinogens
- Substances that can cause cancer are known as carcinogens.
- The process of cancer development is called carcinogenesis.
- Certain carcinogenic chemicals are associated with an increased risk of specific cancers due to chronic exposure.
- One of the most potent carcinogens in humans is benzo[a]pyrene, a compound found in cigarette smoke.
Viruses and Bacteria
- Certain viruses and bacteria have also been associated with the initiation and promotion of tumor growth.
- Some viruses cause cancer directly by affecting cell division while other viruses cause cancer by causing chronic inflammation or reducing immune system function.
Chronic Inflammation
- Chronic inflammation is an important factor in tumor development.
- Inflammation can lead to altered behavior of cells, stimulation of blood vessel growth (angiogenesis) and tissue remodeling.
- Markers of inflammation correlate with a worse prognosis for cancer patients.
- 1 Urry, L. A., Cain, M. L., Wasserman, S. A., Minorsky, P. V., & Reece, J. B. (2017). Campbell Biology (11th ed.). Pearson.
- 2 Weinberg, RA. "Finding the Anti-Oncogene." Scientific American (1988). 259(3): 44-51. [PUBMED]
- 3ab Yamagiwa K, Ichikawa K. Experimental Study of the Pathogenesis of Carcinoma. J Cancer Res 3:1-29 (1918). [http://caonline.amcancersoc.org/cgi/content/abstract/27/3/174]
- 4abcd Troll W, Wiesner R. The role of oxygen radicals as a possible mechanism of tumor promotion. Annu Rev Pharmacol Toxicol. 1985;25:509-28. [PUBMED]
- 5abcde Pitot, H.C., Goldsworthy, T., Moran, S. The natural history of carcinogenesis: Implications of experimental carcinogenesis in the genesis of human cancer. Journal of Supramolecular Structure and Cellular Biochemistry; Volume 17, Issue 2 , Pages 133 146. Published Online: 19 Feb 2004.
- 6 Alberts, B., Johnson, A., Lewis, J., Raff, M., Roberts, K., & Walter, P. Molecular Biology of the Cell; Fourth Edition. 23. Cancer. Garland Science; NY. 2002.
- 7abc Mackenzie IC. "Cancer Stem Cells" Annals of Oncology. 2008 Jul;19 Suppl 5:v40-3. [PUBMED]
- 8abcd Boman BM, Wicha MS. "Cancer Stem Cells: A Step Toward the Cure" Journal of Clinical Oncology. 2008 Jun 10;26(17):2795-9. [PUBMED]
- 9 Stadtfeld M, Nagaya M, Utikal J, Weir G, Hochedlinger K. "Induced Pluripotent Stem Cells Generated Without Viral Integration." Science. 2008 Sep 25. [PUBMED]
- 10 Lee CJ, Dosch J, Simeone DM. "Pancreatic Cancer Stem Cells." Journal of Clinical Oncology (2008); 26(17):2806-12 [PUBMED]
- 11ab Pan CX, Zhu W, Cheng L. "Implications of cancer stem cells in the treatment of cancer." Future Oncology. 2006 Dec;2(6):723-31. [PUBMED]
- 12 Powers, Virginia. "Napabucasin Clinically Active in Both Pancreatic and Colon Cancer." OncLive (2017). [ONCLIVE]
- 13 BH O'Neil, et al. "LBA-003 Phase 1b/II study of cancer stemness inhibitor napabucasin in combination with FOLFIRI +/− bevacizumab (bev) in metastatic colorectal cancer (mCRC) patients (pts)." Annals of Oncology (2017). [ANN ONCOL]
- 14 Huang, X., Jin, A., Wang, X., Gao, X., Xu, H., Chung, M., … Jiang, L. (2021). Napabucasin Induces Mouse Bone Loss by Impairing Bone Formation via STAT3. Frontiers in Cell and Developmental Biology, 9, 648866. http://doi.org/10.3389/fcell.2021.648866 (Original work published December 2021) [PUBMED]
- 15 De Francesco, E. (2017). Vitamin C and Doxycycline: A synthetic lethal combination therapy targeting metabolic flexibility in cancer stem cells (CSCs). Oncotarget, 8(40), 67269–67286. http://doi.org/10.18632/oncotarget.18428 (Original work published September 2017) [PUBMED]